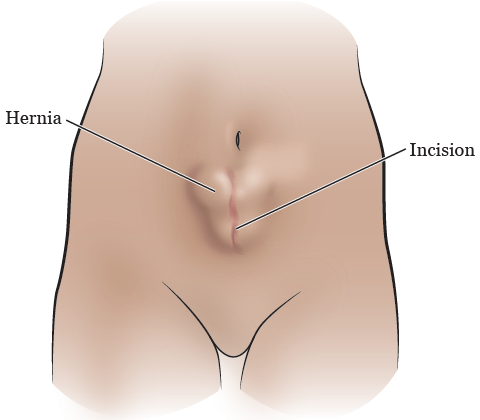
An incisional hernia occurs when tissue protrudes through a weakened area in a surgical incision or scar from a previous surgery. Despite advancements in surgical techniques, these hernias can develop, posing challenges and discomfort for patients. Exploring the causes, symptoms, and available treatment options for incisional hernias is crucial in managing and addressing this medical condition effectively.
Understanding Incisional Hernias
What Is an Incisional Hernia?
An incisional hernia occurs when tissue, such as part of the intestine, protrudes through an opening or weakness in the abdominal muscles at or near the site of a previous surgical incision. This type of hernia can develop weeks, months, or even years after abdominal surgery when the weakened area fails to heal properly, allowing tissues to push through.
Types of Hernias and Their Differences
- Inguinal Hernia: This is the most common type of hernia, occurring in the groin area. It happens when tissue, often part of the intestine, pushes through a weak spot in the lower abdominal muscles.
- Incisional Hernia: As mentioned, this type of hernia occurs at or near the site of a previous surgical incision where the abdominal muscles weaken or separate, allowing tissues to protrude.
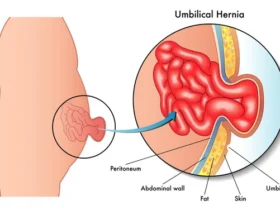
- Umbilical Hernia: Umbilical hernias appear near the belly button when abdominal tissues push through a weakened area in the abdominal wall around the navel.
- Hiatal Hernia: This type of hernia involves the upper stomach protruding through the diaphragm into the chest cavity via an opening called the hiatus. It’s more related to the digestive system than abdominal muscles.
Each hernia type has distinct characteristics based on its location, causes, and potential risks. Incisional hernias specifically occur due to weakened or inadequately healed abdominal muscles post-surgery, leading to tissue protrusion.
Incisional hernias are a specific type of hernia that develops at or near a previous surgical incision site due to weakened abdominal muscles. Understanding the differences between hernia types helps in recognizing and addressing these conditions appropriately based on their distinct characteristics and locations within the body.
Causes of Incisional Hernias
Common Causes of Incisional Hernias:
- Poor Wound Healing: Inadequate healing of the surgical incision site can lead to weakened abdominal muscles, allowing tissues to protrude through the weakened area.
- Increased Intra-Abdominal Pressure: Activities or conditions that increase intra-abdominal pressure, such as heavy lifting, chronic coughing, obesity, or pregnancy, can strain the weakened abdominal wall and contribute to hernia formation.
- Surgical Techniques: Factors related to the surgical procedure itself, such as excessive tension on the incision site during closure, infection, or the type of incision made, can influence the risk of an incisional hernia.
Risk Factors for Incisional Hernias:
- Previous Abdominal Surgery: Any prior abdominal surgeries, especially if the incisional closure was under tension or if complications like wound infections occurred, increase the risk of an incisional hernia.
- Obesity: Excess body weight puts added stress on the abdominal muscles, increasing the risk of hernia development.
- Age: Older individuals may have weaker abdominal muscles, making them more susceptible to hernias.
- Chronic Conditions: Chronic coughing due to conditions like chronic obstructive pulmonary disease (COPD) or ongoing straining due to constipation can raise the risk.
- Smoking: Smoking impedes proper wound healing, potentially increasing the risk of an incisional hernia.
- Genetics: Some individuals may have a genetic predisposition to weakened connective tissues, which can contribute to hernia formation.
Incisional hernias commonly result from poor wound healing at a previous surgical incision site or increased pressure on weakened abdominal muscles. Several factors, including previous surgeries, obesity, age, lifestyle habits, and certain health conditions, heighten the risk of developing an incisional hernia. Understanding these causes and risk factors helps in preventive measures and early detection of potential hernias.
Symptoms of Incisional Hernias
Recognizing Signs and Symptoms:
- Visible Bulge: A noticeable bulge or lump near or at the site of a previous surgical incision, particularly when standing, coughing, or straining, is a common symptom.
- Discomfort or Pain: Some individuals may experience discomfort, pain, or a dragging sensation at the hernia site, especially during physical activity or when straining.
- Swelling or Redness: Swelling, redness, or tenderness around the hernia site might be present, especially if the hernia becomes incarcerated or strangulated.
- Digestive Issues: In some cases, an incisional hernia might cause digestive problems, such as nausea, vomiting, or difficulty passing stools, if it obstructs the intestines.
Potential Complications:
- Incarceration: The hernia sac becomes stuck in the opening, causing a persistent bulge that can’t be pushed back in. This may lead to severe pain and discomfort.
- Strangulation: A severe complication where the blood supply to the herniated tissue is cut off, causing tissue damage. It’s a medical emergency requiring immediate attention.
- Bowel Obstruction: If the herniated intestine becomes blocked, it can lead to nausea, vomiting, abdominal distension, and severe abdominal pain.
- Perforation or Infection: In rare cases, incarcerated or strangulated hernias can cause tissue damage, leading to perforation or infection, requiring urgent medical intervention.
Symptoms of incisional hernias often involve a visible bulge, discomfort or pain, and occasionally digestive issues. Recognizing these signs is crucial for early detection and timely intervention. Complications such as incarceration, strangulation, bowel obstruction, and potential tissue damage underscore the importance of prompt medical evaluation and treatment if symptoms appear or worsen. Seeking immediate medical attention for severe pain, a tender bulge that cannot be pushed back in, or signs of obstruction or strangulation is critical to avoid serious complications.
Diagnosis and Imaging for Incisional Hernias
Physical Examination and Medical History:
- Physical Examination: A healthcare provider examines the abdomen, focusing on the site of the previous surgical incision for any visible bulges, tenderness, or signs of herniation. The patient may be asked to cough or strain to help identify the hernia.
- Medical History: The medical history includes details about previous surgeries, abdominal injuries, and any symptoms related to hernias, such as pain, discomfort, or changes in bowel habits.
Imaging Tests for Diagnosis:
- Ultrasound: Often used as an initial imaging test, ultrasound helps visualize the hernia and assess its size, location, and potential complications.
- CT Scan (Computed Tomography): CT scans provide detailed cross-sectional images of the abdomen, helping to identify the hernia, its contents, and any complications like incarceration or strangulation.
- MRI (Magnetic Resonance Imaging): MRI scans offer detailed images without radiation and can provide information about the hernia’s characteristics and its impact on surrounding tissues.
- X-ray: While less commonly used, X-rays may help identify complications like bowel obstruction or perforation associated with hernias.
Diagnosis of incisional hernias involves a thorough physical examination focusing on the abdomen and the site of the previous surgical incision. Healthcare providers rely on a combination of medical history and physical findings to suspect a hernia. Imaging tests such as ultrasound, CT scans, MRI scans, and occasionally X-rays help confirm the diagnosis, assess the hernia’s characteristics, size, and any potential complications, aiding in the development of an appropriate treatment plan.
Treatment Options for Incisional Hernias
Non-Surgical Approaches:
- Watchful Waiting: Small, asymptomatic hernias might be monitored without immediate intervention, especially if they don’t cause discomfort or complications.
- Supportive Measures: Wearing a supportive abdominal binder or truss might help reduce discomfort and support the hernia but does not cure it.
Surgical Repair Techniques:
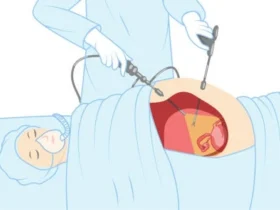
- Open Hernia Repair: Involves making an incision directly over the hernia site to push the bulging tissue back into place and repair the weakened abdominal wall using stitches or synthetic mesh.
- Laparoscopic Hernia Repair: A minimally invasive approach involving several small incisions through which a laparoscope and specialized instruments are used to repair the hernia, often utilizing mesh reinforcement.
- Robotic-Assisted Hernia Repair: Similar to laparoscopic repair but with the assistance of robotic technology for enhanced precision in complex cases.
Choosing the Right Treatment:
- Size and Symptoms: The size of the hernia and the presence of symptoms like pain or discomfort often influence the decision for surgical repair.
- Patient’s Health Status: The patient’s overall health, any existing medical conditions, and the risks associated with surgery are important considerations when choosing treatment.
- Surgeon’s Recommendation: A qualified surgeon’s assessment and recommendation based on the hernia’s characteristics, potential complications, and the patient’s individual situation play a significant role in determining the appropriate treatment.
The treatment approach for incisional hernias varies based on the hernia’s size, symptoms, and the patient’s overall health. Non-surgical options like watchful waiting or supportive measures may be suitable for small, asymptomatic hernias. However, surgical repair, either through open, laparoscopic, or robotic-assisted techniques, is often the primary treatment for symptomatic or larger hernias. Collaborating closely with a skilled surgeon helps in choosing the most appropriate treatment method tailored to the individual’s needs and ensuring optimal outcomes.
Recovery and Postoperative Care for Incisional Hernia Repair
Post-Surgery Recovery Timeline:
- Immediate Post-Op: Patients typically spend a short time in the recovery room before being discharged on the same day or the following day for minimally invasive repairs. Open repairs might require a longer hospital stay.
- First Few Days: Initial days involve managing discomfort, following prescribed pain medications, and limiting activities. Avoiding heavy lifting and strenuous activities is crucial.
- First Week: Patients can gradually resume light activities as tolerated. Follow specific instructions regarding wound care, diet, and medication.
- Several Weeks: Healing continues over the next few weeks. Patients should avoid heavy lifting or activities that strain the abdominal area until cleared by the surgeon.
- Follow-Up Appointments: Scheduled follow-up appointments with the surgeon are essential for monitoring healing, removing stitches if necessary, and assessing overall progress.
Recovery Tips and Complication Warning Signs:
- Manage Discomfort: Follow the prescribed pain medications and apply ice packs as advised to manage discomfort and reduce swelling.
- Wound Care: Keep the incision area clean and dry, following the surgeon’s instructions for wound care to prevent infection.
- Activity Level: Gradually increase activity levels as guided by the surgeon, but avoid strenuous activities or heavy lifting until approved.
- Complication Warning Signs: Watch for signs of complications such as increasing pain, redness, swelling, fever, persistent vomiting, or inability to pass gas or stool. Contact the surgeon immediately if any of these symptoms occur.
The recovery timeline for incisional hernia repair involves gradual healing over several weeks. Following postoperative instructions regarding wound care, activity levels, pain management, and attending follow-up appointments is crucial for a smooth recovery. Monitoring for signs of complications and seeking immediate medical attention if any warning signs appear is vital to prevent potential complications and ensure a successful recovery.
Preventing Incisional Hernia Recurrence
Lifestyle Changes and Prevention Measures:
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight reduces stress on the abdominal muscles, decreasing the risk of hernia recurrence.
- Avoid Heavy Lifting: Minimize heavy lifting and strenuous activities, especially during the initial recovery period and beyond, to prevent excessive strain on the abdominal muscles.
- Proper Nutrition and Exercise: Follow a balanced diet and engage in regular exercise to strengthen abdominal muscles and maintain overall health.
- Quit Smoking: Smoking impedes proper wound healing and increases the risk of complications. Quitting smoking can contribute to better healing outcomes.
Follow-Up Care and Monitoring:
- Regular Check-Ups: Attend scheduled follow-up appointments with the surgeon to monitor the healing process, assess the surgical site, and identify any potential issues early on.
- Abdominal Support: If recommended by the surgeon, using abdominal binders or support garments during recovery or while engaging in activities might help prevent excessive strain on the surgical site.
- Early Intervention for Symptoms: Report any unusual symptoms, pain, discomfort, or changes in the surgical site to the surgeon promptly to prevent potential complications or hernia recurrence.
Preventing incisional hernia recurrence involves lifestyle changes such as maintaining a healthy weight, avoiding heavy lifting, and following proper nutrition and exercise. Regular follow-up care, attending check-ups, and promptly addressing any concerning symptoms or changes in the surgical site with the surgeon contribute to monitoring and preventing potential complications or hernia recurrence. Combining these preventive measures with ongoing attention to overall health helps reduce the risk of incisional hernia recurrence and promotes better long-term outcomes.
You may want to read about : Liposuction cost in Dubai and 3 main factors affecting it
When to Seek Medical Help
Indications for Urgent Medical Attention
Seek urgent medical attention if you experience any of the following indications after incisional hernia repair:
- Severe Pain: Intense or worsening pain at the surgical site that doesn’t subside with prescribed pain medications.
- Fever: A persistent fever, especially accompanied by chills or sweating, could indicate an infection.
- Redness, Swelling, or Warmth: Increasing redness, swelling, warmth, or tenderness around the incision site may indicate an infection or other complications.
- Nausea and Vomiting: Persistent nausea or vomiting could signal complications such as bowel obstruction.
- Bulge or Protrusion: A noticeable bulge or protrusion at the surgical site that doesn’t recede or is associated with severe discomfort.
- Inability to Pass Gas or Stool: A complete inability to pass gas or stool could suggest a blockage, requiring immediate medical attention.
- Difficulty Breathing or Chest Pain: Difficulty breathing or chest pain might indicate serious complications such as a pulmonary embolism and require immediate evaluation.
Any significant or concerning changes in the surgical site, severe pain, signs of infection, or symptoms indicating potential complications warrant prompt medical evaluation. It’s essential to contact your healthcare provider or seek emergency medical care if you observe any of these indications after incisional hernia repair.
FAQs about Incisional Hernias
How much does hernia surgery cost in UAE?
Hernia surgery costs in the UAE can vary based on several factors, including the type of surgery, the hospital or clinic, the surgeon’s expertise, and any additional treatments or facilities required. Costs may include surgeon fees, hospital charges, anesthesia, and post-operative care. It’s advisable to consult with healthcare providers or hospitals directly for specific pricing details.
What is the success rate of incisional hernia repair?
The success rate of incisional hernia repair surgery is generally high. Success is measured by the reduction of hernia recurrence and alleviation of symptoms. However, success rates may vary based on the size of the hernia, the surgical technique used, the patient’s overall health, and the surgeon’s skill. Skilled surgeons and appropriate post-operative care significantly contribute to successful outcomes.
How urgent is an incisional hernia?
While some incisional hernias may not cause immediate discomfort or complications, others may require urgent attention. Incisional hernias can become urgent if they cause severe pain, become incarcerated (trapped outside the abdominal wall), or strangulated (where the blood supply to the herniated tissue is compromised). These situations require immediate medical attention to prevent serious complications.
What is the best repair for an incisional hernia?
The “best” repair for an incisional hernia depends on various factors, including the size and location of the hernia, the patient’s overall health, and the surgeon’s expertise. Surgical options include open repair, laparoscopic repair, or robotic-assisted repair. The choice of repair technique is individualized based on the specific characteristics of the hernia and the patient’s condition. Consulting with a skilled surgeon helps determine the most suitable repair method for an incisional hernia.



Leave a Reply