Overview Of Anogenital pruritus
Anogenital pruritus refers to persistent itching in the anal and genital regions, a condition that can cause significant discomfort and distress. It is a symptom rather than a disease itself and can result from a wide range of underlying causes, including infections, skin conditions, systemic diseases, or psychological factors. The itching may be localized to the anus, vulva, or scrotum and can range from mild to severe, often worsening at night or after sweating. Chronic scratching can lead to skin thickening, discoloration, and secondary infections, further complicating the condition. Anogenital pruritus can affect individuals of any age or gender, though certain causes may be more prevalent in specific populations. Proper diagnosis and treatment are essential to address the underlying cause and alleviate symptoms.
Symptoms of Anogenital pruritus
- The primary symptom of anogenital pruritus is itching, which may be accompanied by other signs depending on the underlying cause. Common symptoms include:
- Itching: Persistent and often intense, particularly at night.
- Redness and Inflammation: The affected area may appear red and swollen.
- Skin Changes: Thickening (lichenification), scaling, or cracking of the skin due to chronic scratching.
- Pain or Burning: Discomfort during urination, bowel movements, or sexual activity.
- Discharge: In cases of infection, there may be abnormal vaginal or penile discharge.
- Bleeding: Scratching can cause small tears or bleeding.
- Secondary Infections: Bacterial or fungal infections due to broken skin. Symptoms can vary in severity and may fluctuate over time.
Causes of Anogenital pruritus
- Anogenital pruritus can arise from a variety of causes, which can be broadly categorized into local and systemic factors. Common causes include:
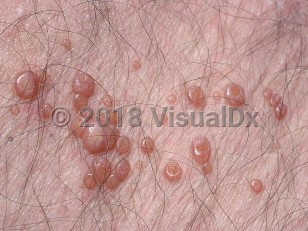
- Infections: Fungal (e.g., candidiasis), bacterial (e.g., streptococcal infections), parasitic (e.g., pinworms, scabies), or viral (e.g., herpes).
- Skin Conditions: Eczema, psoriasis, lichen sclerosus, or contact dermatitis.
- Hygiene Factors: Excessive washing, use of harsh soaps, or inadequate drying of the area.
- Systemic Diseases: Diabetes, liver or kidney disorders, thyroid dysfunction, or iron deficiency anemia.
- Sexually Transmitted Infections (STIs): Such as gonorrhea, chlamydia, or trichomoniasis.
- Allergic Reactions: To latex, spermicides, or personal care products.
- Psychological Factors: Stress, anxiety, or obsessive-compulsive behaviors.
- Hemorrhoids or Fissures: Anal conditions that can cause irritation and itching. Identifying the underlying cause is crucial for effective treatment.
Risk Factors of Anogenital pruritus
- Several factors can increase the likelihood of developing anogenital pruritus:
- Poor Hygiene: Inadequate cleaning or excessive use of irritants.
- Obesity: Excess moisture and friction in skin folds can promote itching.
- Diabetes: High blood sugar levels can increase the risk of infections.
- Weakened Immune System: Conditions like HIV or use of immunosuppressive medications.
- Sexual Activity: Increased risk of STIs or irritation from lubricants or condoms.
- Age: Older adults may experience dryness and thinning of the skin.
- Pregnancy: Hormonal changes and increased moisture can contribute to itching.
- Pre-existing Skin Conditions: Such as eczema or psoriasis. Understanding these risk factors can help in prevention and early intervention.
Prevention of Anogenital pruritus
- Preventing anogenital pruritus involves maintaining proper hygiene and avoiding known triggers. Key preventive measures include:
- Proper Hygiene: Gentle cleaning with mild, fragrance-free soaps and thorough drying.
- Avoiding Irritants: Steering clear of harsh chemicals, perfumed products, or tight clothing.
- Moisturizing: Regularly applying hypoallergenic moisturizers to prevent dryness.
- Managing Underlying Conditions: Controlling diabetes, thyroid disorders, or other systemic diseases.
- Safe Sexual Practices: Using protection to reduce the risk of STIs.
- Stress Management: Practicing relaxation techniques to reduce stress-related itching.
- Regular Check-ups: Monitoring for infections or skin changes. By incorporating these strategies, individuals can reduce the risk of developing anogenital pruritus.
Prognosis of Anogenital pruritus
- The prognosis for anogenital pruritus depends on the underlying cause and the effectiveness of treatment. In many cases, symptoms can be effectively managed with appropriate therapy, leading to significant relief and improved quality of life. However, chronic or recurrent cases may require long-term management and lifestyle adjustments. Early diagnosis and treatment are crucial to prevent complications such as skin thickening, infections, or emotional distress. With proper care, most individuals can achieve symptom control and prevent recurrence.
Complications of Anogenital pruritus
- If left untreated, anogenital pruritus can lead to several complications:
- Skin Infections: Bacterial or fungal infections due to broken skin from scratching.
- Chronic Lichenification: Thickened, leathery skin from prolonged scratching.
- Emotional Distress: Persistent itching can cause anxiety, depression, or sleep disturbances.
- Scarring: Chronic inflammation and scratching can lead to permanent skin changes.
- Secondary Conditions: Such as vulvodynia or proctitis, depending on the affected area.
- Social Impact: Discomfort and embarrassment can affect relationships and daily activities. Addressing these complications requires a comprehensive approach, including medical treatment and psychological support.
Related Diseases of Anogenital pruritus
- Anogenital pruritus is often associated with other conditions that affect the skin or systemic health. Related diseases include:
- Candidiasis: A fungal infection that can cause itching and discharge.
- Psoriasis: An autoimmune condition causing scaly, inflamed skin.
- Lichen Sclerosus: A chronic skin condition affecting the genital area.
- Hemorrhoids: Swollen blood vessels in the anal region that can cause itching.
- Diabetes: High blood sugar levels can increase the risk of infections and itching.
- Sexually Transmitted Infections (STIs): Such as herpes, gonorrhea, or trichomoniasis.
- Eczema: A chronic inflammatory skin condition characterized by dryness and itching. Understanding these related diseases can help in managing anogenital pruritus more effectively, as they may share common triggers or require similar treatment approaches.
Treatment of Anogenital pruritus
Treatment for anogenital pruritus focuses on addressing the underlying cause and relieving symptoms. Common approaches include: 1. **Topical Corticosteroids**: To reduce inflammation and itching. 2. **Antifungal or Antibacterial Creams**: For infections caused by fungi or bacteria. 3. **Antihistamines**: To alleviate itching, especially at night. 4. **Moisturizers**: To restore the skin barrier and prevent dryness. 5. **Cool Compresses**: To soothe irritated skin. 6. **Behavioral Modifications**: Avoiding scratching, wearing loose clothing, and maintaining proper hygiene. 7. **Systemic Medications**: Oral antibiotics, antifungals, or antiparasitics for severe or widespread infections. 8. **Counseling**: For cases linked to stress or psychological factors. Treatment plans are tailored to the individual’s specific needs and underlying cause.
Generics For Anogenital pruritus
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Hydrocortisone 1% Topical
Hydrocortisone 1% Topical

Cinchocaine Hydrochloride 0.5% + Esculin 1% + Hydrocortisone + Neomycin Sulphate (Rectal prep)
Cinchocaine Hydrochloride 0.5% + Esculin 1% + Hydrocortisone + Neomycin Sulphate (Rectal prep)

Betamethasone 0.05% + Lidocaine Hydrochloride 2.5%+ Phenylephrine Hydrochloride 0.1% (Rectal prep)
Betamethasone 0.05% + Lidocaine Hydrochloride 2.5%+ Phenylephrine Hydrochloride 0.1% (Rectal prep)

Bacitracin Zinc + Neomycin Sulphate + Polymixin B topical
Bacitracin Zinc + Neomycin Sulphate + Polymixin B topical

Betamethasone + Clotrimazole + Gentamicin Topical
Betamethasone + Clotrimazole + Gentamicin Topical

Capsaicin 0.025% topical
Capsaicin 0.025% topical

Hydrocortisone + Lidocaine rectal prep
Hydrocortisone + Lidocaine rectal prep

Triamcinolone Acetonide 0.1% Topical
Triamcinolone Acetonide 0.1% Topical

Hydrocortisone 1% Topical
Hydrocortisone 1% Topical

Cinchocaine Hydrochloride 0.5% + Esculin 1% + Hydrocortisone + Neomycin Sulphate (Rectal prep)
Cinchocaine Hydrochloride 0.5% + Esculin 1% + Hydrocortisone + Neomycin Sulphate (Rectal prep)

Betamethasone 0.05% + Lidocaine Hydrochloride 2.5%+ Phenylephrine Hydrochloride 0.1% (Rectal prep)
Betamethasone 0.05% + Lidocaine Hydrochloride 2.5%+ Phenylephrine Hydrochloride 0.1% (Rectal prep)

Bacitracin Zinc + Neomycin Sulphate + Polymixin B topical
Bacitracin Zinc + Neomycin Sulphate + Polymixin B topical

Betamethasone + Clotrimazole + Gentamicin Topical
Betamethasone + Clotrimazole + Gentamicin Topical

Capsaicin 0.025% topical
Capsaicin 0.025% topical

Hydrocortisone + Lidocaine rectal prep
Hydrocortisone + Lidocaine rectal prep

Triamcinolone Acetonide 0.1% Topical
Triamcinolone Acetonide 0.1% Topical