Overview Of Susceptible infections
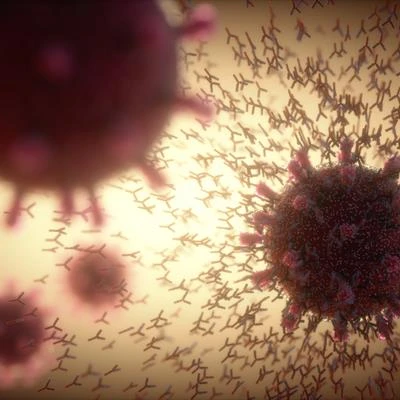
Susceptible infections refer to infections that occur in individuals with an increased vulnerability to pathogens due to compromised immune systems, underlying health conditions, or environmental factors. These infections can be caused by bacteria, viruses, fungi, or parasites and often result in more severe or recurrent illnesses compared to infections in healthy individuals. Susceptible populations include those with immunodeficiency disorders (e.g., HIV/AIDS, primary immunodeficiencies), chronic diseases (e.g., diabetes, cancer), or those undergoing treatments that suppress the immune system (e.g., chemotherapy, corticosteroids). Additionally, environmental factors such as poor sanitation, malnutrition, and exposure to pollutants can increase susceptibility. Early diagnosis, targeted treatment, and preventive measures are essential to manage these infections and improve outcomes.
Symptoms of Susceptible infections
- The symptoms of susceptible infections vary depending on the type of pathogen and the site of infection. Common symptoms include fever, fatigue, and generalized weakness, which are often more severe in immunocompromised individuals. Respiratory infections may cause cough, shortness of breath, and chest pain, while gastrointestinal infections can lead to diarrhea, vomiting, and abdominal pain. Skin and soft tissue infections may present with redness, swelling, and pus formation. In severe cases, systemic symptoms such as sepsis, organ failure, or neurological complications can occur. Early recognition of symptoms is critical for prompt diagnosis and treatment, particularly in high-risk populations.
Causes of Susceptible infections
- Susceptible infections are caused by a wide range of pathogens, including bacteria (e.g., *Staphylococcus aureus*, *Pseudomonas aeruginosa*), viruses (e.g., cytomegalovirus, influenza), fungi (e.g., *Candida*, *Aspergillus*), and parasites (e.g., *Toxoplasma gondii*). The primary factor contributing to susceptibility is a compromised immune system, which can result from congenital or acquired immunodeficiency disorders, chronic illnesses, or immunosuppressive therapies. Environmental factors, such as poor hygiene, malnutrition, and exposure to contaminated water or air, also play a significant role. Additionally, lifestyle factors like smoking, alcohol abuse, and lack of access to healthcare can increase vulnerability. Understanding the underlying causes is crucial for effective prevention and treatment.
Risk Factors of Susceptible infections
- Several factors increase the risk of susceptible infections. Immunodeficiency disorders, such as HIV/AIDS, primary immunodeficiencies, or secondary immunodeficiencies caused by chemotherapy or corticosteroids, are significant risk factors. Chronic diseases, including diabetes, cancer, and chronic kidney disease, impair the body's ability to fight infections. Environmental factors, such as poor sanitation, malnutrition, and exposure to pollutants, further increase susceptibility. Lifestyle factors, such as smoking, alcohol abuse, and lack of access to healthcare, also contribute to the risk. Addressing these risk factors through medical management, lifestyle changes, and public health interventions is essential for reducing the incidence of susceptible infections.
Prevention of Susceptible infections
- Preventing susceptible infections involves a combination of medical management, lifestyle changes, and public health measures. Vaccination against common pathogens, such as influenza, pneumococcus, and hepatitis B, is highly effective in reducing the incidence of infections. For immunocompromised individuals, prophylactic antibiotics or antiviral medications may be recommended. Good hygiene practices, such as regular handwashing and proper food preparation, can reduce the risk of infection. Addressing underlying conditions, such as diabetes or HIV/AIDS, through optimal medical management is essential for preventing recurrent infections. Public health initiatives, such as improving sanitation and access to clean water, play a vital role in reducing the burden of susceptible infections.
Prognosis of Susceptible infections
- The prognosis for susceptible infections varies depending on the causative pathogen, the severity of the infection, and the patient's overall health. With appropriate treatment, many individuals can achieve significant improvement in symptoms and recovery. However, immunocompromised patients or those with severe underlying conditions may experience prolonged or recurrent infections, leading to chronic health issues or life-threatening complications. Early diagnosis, adherence to treatment, and regular follow-up care are essential for improving prognosis and preventing long-term complications. Addressing underlying conditions and risk factors is key to achieving better outcomes.
Complications of Susceptible infections
- If left untreated or inadequately managed, susceptible infections can lead to serious complications. Systemic infections, such as sepsis or multi-organ failure, can be life-threatening. Chronic infections can result in long-term damage to affected organs, such as the lungs, liver, or kidneys. Immunocompromised individuals are at higher risk for opportunistic infections, which can cause severe or unusual presentations. Recurrent infections can lead to a decline in overall health, including weight loss, fatigue, and reduced quality of life. Early diagnosis and treatment are crucial to minimize the risk of these complications and preserve organ function.
Related Diseases of Susceptible infections
- Susceptible infections are closely related to other conditions that compromise the immune system or increase vulnerability to pathogens. These include immunodeficiency disorders, such as HIV/AIDS and primary immunodeficiencies, as well as chronic diseases like diabetes, cancer, and chronic kidney disease. Opportunistic infections, such as *Pneumocystis* pneumonia or cytomegalovirus, are common in immunocompromised individuals. Other related conditions include sepsis, which can result from severe infections, and chronic infections, such as tuberculosis or hepatitis. Understanding these relationships is essential for accurate diagnosis, effective treatment, and comprehensive prevention of susceptible infections.
Treatment of Susceptible infections
The treatment of susceptible infections depends on the causative pathogen and the patient's underlying condition. Bacterial infections are typically treated with antibiotics, while antiviral medications may be used for viral infections. Fungal infections require antifungal therapy, and parasitic infections are treated with antiparasitic drugs. In immunocompromised individuals, treatment may also include immunomodulatory therapies, such as immunoglobulin replacement or growth factors. Supportive care, including hydration, pain management, and nutritional support, is essential for all patients. Early and targeted treatment is crucial to prevent complications and improve outcomes.
Generics For Susceptible infections
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Ampicillin
Ampicillin

Cefadroxil
Cefadroxil

Cefdinir
Cefdinir

Cefditoren
Cefditoren

Cefetamet Pivoxil Hydrochloride
Cefetamet Pivoxil Hydrochloride

Cefixime
Cefixime

Cefpirome
Cefpirome

Cefprozil
Cefprozil

Cefuroxime
Cefuroxime

Cefuroxime + Clavulanic Acid
Cefuroxime + Clavulanic Acid

Cephradine
Cephradine

Imipenem + Cilastatin
Imipenem + Cilastatin

Doxycycline
Doxycycline

Erythromycin
Erythromycin

Gatifloxacin
Gatifloxacin

Gentamicin
Gentamicin

Oxytetracycline
Oxytetracycline

Pefloxacin
Pefloxacin

Roxithromycin
Roxithromycin

Spiramycine
Spiramycine

Ampicillin
Ampicillin

Cefadroxil
Cefadroxil

Cefdinir
Cefdinir

Cefditoren
Cefditoren

Cefetamet Pivoxil Hydrochloride
Cefetamet Pivoxil Hydrochloride

Cefixime
Cefixime

Cefpirome
Cefpirome

Cefprozil
Cefprozil

Cefuroxime
Cefuroxime

Cefuroxime + Clavulanic Acid
Cefuroxime + Clavulanic Acid

Cephradine
Cephradine

Imipenem + Cilastatin
Imipenem + Cilastatin

Doxycycline
Doxycycline

Erythromycin
Erythromycin

Gatifloxacin
Gatifloxacin

Gentamicin
Gentamicin

Oxytetracycline
Oxytetracycline

Pefloxacin
Pefloxacin

Roxithromycin
Roxithromycin

Spiramycine
Spiramycine