Overview Of Chronic obstructive pulmonary disease (COPD)
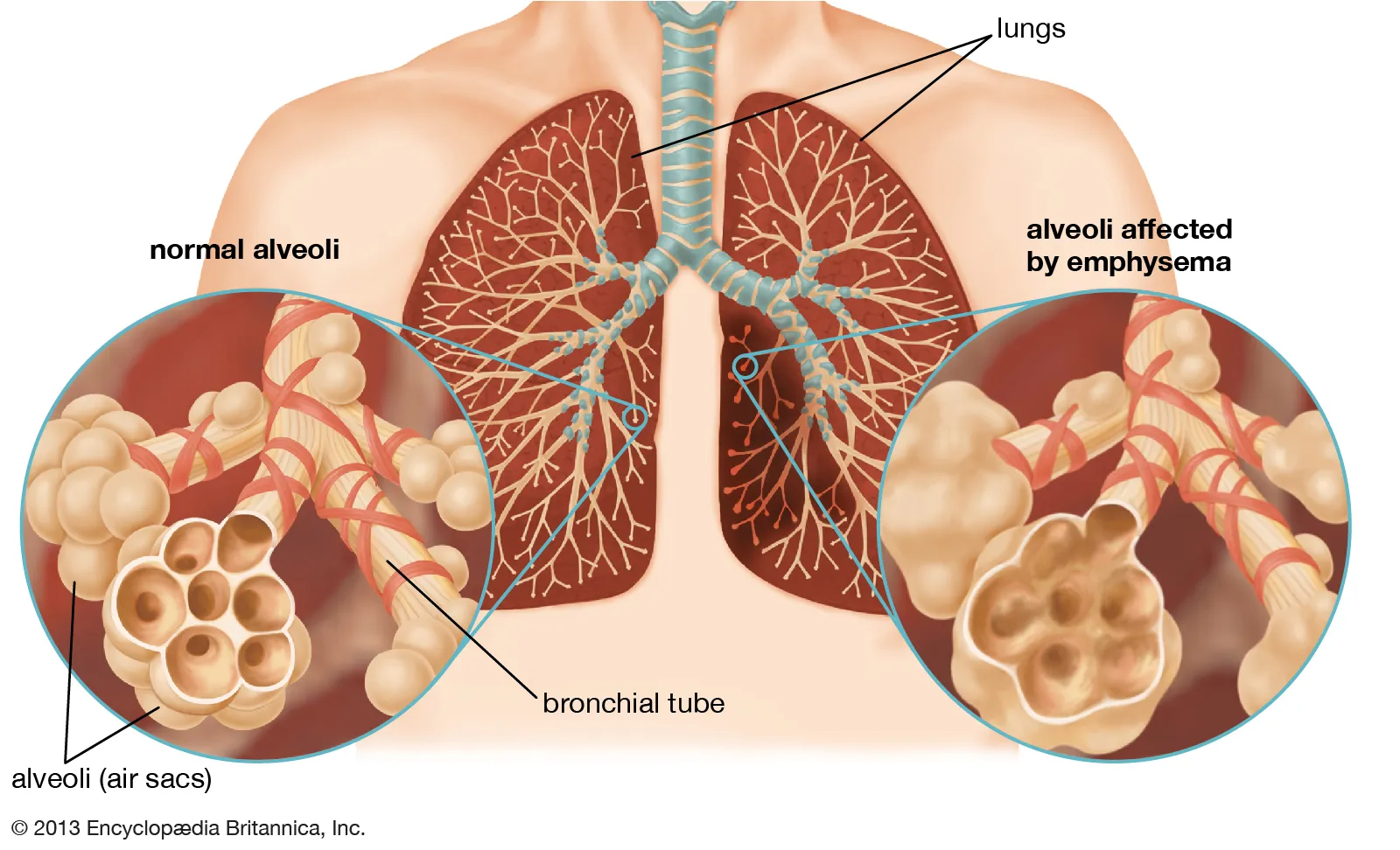
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities. It is primarily caused by long-term exposure to harmful gases or particulate matter, most commonly from cigarette smoke. COPD encompasses two main conditions: chronic bronchitis, which involves long-term inflammation of the airways, and emphysema, which involves damage to the air sacs (alveoli) in the lungs. Symptoms include chronic cough, shortness of breath, wheezing, and excess mucus production. COPD is a leading cause of morbidity and mortality worldwide, significantly impacting quality of life. While there is no cure, early diagnosis and management can slow disease progression and improve symptoms.
Symptoms of Chronic obstructive pulmonary disease (COPD)
- The symptoms of COPD develop gradually and worsen over time. Common symptoms include:
- Chronic Cough: Often producing mucus (sputum).
- Shortness of Breath (Dyspnea): Especially during physical activity.
- Wheezing: A whistling sound during breathing.
- Chest Tightness: A sensation of pressure or discomfort.
- Frequent Respiratory Infections: Such as bronchitis or pneumonia.
- Fatigue: Due to reduced oxygen levels and increased effort to breathe.
- Weight Loss: In advanced stages, due to difficulty eating and increased energy expenditure.
- Bluish Lips or Fingernails (Cyanosis): Indicating low oxygen levels. Symptoms may worsen during exacerbations, often triggered by infections or environmental factors.
Causes of Chronic obstructive pulmonary disease (COPD)
- COPD is primarily caused by long-term exposure to irritants that damage the lungs and airways. Key causes include:
- Cigarette Smoking: The leading cause, responsible for about 85-90% of cases.
- Environmental Exposures: Prolonged exposure to air pollution, chemical fumes, or dust.
- Genetic Factors: Alpha-1 antitrypsin deficiency, a rare genetic condition that increases susceptibility.
- Occupational Hazards: Jobs involving exposure to coal dust, silica, or cotton fibers.
- Biomass Fuel Exposure: Common in developing countries due to cooking with wood or dung.
- Recurrent Respiratory Infections: Frequent lung infections can contribute to lung damage.
- Aging: Natural decline in lung function over time. Understanding these causes helps in prevention and early intervention.
Risk Factors of Chronic obstructive pulmonary disease (COPD)
- Several factors increase the risk of developing COPD:
- Smoking: Current or former smokers are at the highest risk.
- Age: Most commonly diagnosed in individuals over
- Occupational Exposure: Jobs involving dust, chemicals, or fumes.
- Environmental Pollution: Living in areas with high levels of air pollution.
- Genetic Predisposition: Family history of COPD or alpha-1 antitrypsin deficiency.
- Recurrent Lung Infections: Frequent respiratory infections in childhood or adulthood.
- Asthma: Poorly controlled asthma can increase the risk.
- Socioeconomic Status: Limited access to healthcare or clean cooking fuels. Identifying these risk factors can help in prevention and early detection.
Prevention of Chronic obstructive pulmonary disease (COPD)
- Preventing COPD involves reducing exposure to risk factors and maintaining healthy habits. Key preventive measures include:
- Smoking Cessation: Avoiding or quitting smoking is the most effective prevention strategy.
- Reducing Environmental Exposure: Minimizing exposure to air pollution, chemicals, and dust.
- Vaccinations: Getting vaccinated against flu and pneumonia.
- Regular Exercise: To maintain lung function and overall health.
- Healthy Diet: Consuming a balanced diet to support immune function.
- Early Detection: Seeking medical attention for persistent respiratory symptoms.
- Education: Raising awareness about COPD risk factors and prevention. By incorporating these strategies, individuals can reduce the risk of developing COPD.
Prognosis of Chronic obstructive pulmonary disease (COPD)
- The prognosis for COPD varies depending on disease severity, adherence to treatment, and lifestyle changes. While COPD is a progressive disease, early diagnosis and management can significantly slow its progression and improve quality of life. Smoking cessation is the most effective intervention to alter the disease course. However, advanced COPD can lead to significant disability and reduced life expectancy. Regular monitoring, pulmonary rehabilitation, and adherence to treatment are key to achieving the best outcomes.
Complications of Chronic obstructive pulmonary disease (COPD)
- If left untreated or poorly managed, COPD can lead to several complications:
- Respiratory Infections: Increased risk of pneumonia and bronchitis.
- Respiratory Failure: Inability to maintain adequate oxygen levels.
- Heart Problems: Such as pulmonary hypertension or cor pulmonale.
- Lung Cancer: Higher risk due to smoking and chronic inflammation.
- Depression and Anxiety: Due to chronic symptoms and reduced quality of life.
- Weight Loss and Malnutrition: Difficulty eating and increased energy expenditure.
- Exacerbations: Sudden worsening of symptoms, often requiring hospitalization. Addressing these complications requires a comprehensive approach, including medical treatment, lifestyle changes, and psychological support.
Related Diseases of Chronic obstructive pulmonary disease (COPD)
- COPD is often associated with other respiratory and systemic conditions. Related diseases include:
- Asthma: A chronic inflammatory condition of the airways.
- Bronchiectasis: A condition causing permanent enlargement of the airways.
- Pulmonary Fibrosis: Scarring of lung tissue leading to reduced lung function.
- Lung Cancer: Increased risk due to smoking and chronic inflammation.
- Heart Disease: Including pulmonary hypertension and cor pulmonale.
- Osteoporosis: A common comorbidity due to reduced physical activity and steroid use.
- Depression and Anxiety: Often coexisting with chronic respiratory conditions. Understanding these related diseases can help in managing COPD more effectively, as they may share common triggers or require similar treatment approaches.
Treatment of Chronic obstructive pulmonary disease (COPD)
Treatment for COPD focuses on relieving symptoms, slowing disease progression, and improving quality of life. Common approaches include: 1. **Smoking Cessation**: The most critical step in managing COPD. 2. **Bronchodilators**: Inhalers that relax airway muscles (e.g., albuterol, tiotropium). 3. **Inhaled Corticosteroids**: To reduce airway inflammation. 4. **Pulmonary Rehabilitation**: A program of exercise, education, and support. 5. **Oxygen Therapy**: For individuals with low blood oxygen levels. 6. **Vaccinations**: Annual flu shots and pneumococcal vaccines to prevent infections. 7. **Antibiotics**: For treating bacterial respiratory infections. 8. **Lung Volume Reduction Surgery**: In severe cases, to remove damaged lung tissue. 9. **Lung Transplant**: For end-stage COPD in select patients. Treatment plans are tailored to the individual’s disease severity and symptoms.
Generics For Chronic obstructive pulmonary disease (COPD)
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Bambuterol Hydrochloride
Bambuterol Hydrochloride

Beclomethasone Dipropionate
Beclomethasone Dipropionate

Budesonide
Budesonide

Carbocisteine
Carbocisteine

Ipratropium Bromide
Ipratropium Bromide

Ipratropium Bromide + Salbutamol
Ipratropium Bromide + Salbutamol

Levosalbutamol
Levosalbutamol

Roflumilast
Roflumilast

Theophylline
Theophylline

Tiotropium
Tiotropium

Tulobuterol Hydrochloride
Tulobuterol Hydrochloride

Indacaterol
Indacaterol

Doxofylline
Doxofylline

Indacaterol + Glycopyrronium
Indacaterol + Glycopyrronium

Bambuterol Hydrochloride
Bambuterol Hydrochloride

Beclomethasone Dipropionate
Beclomethasone Dipropionate

Budesonide
Budesonide

Carbocisteine
Carbocisteine

Ipratropium Bromide
Ipratropium Bromide

Ipratropium Bromide + Salbutamol
Ipratropium Bromide + Salbutamol

Levosalbutamol
Levosalbutamol

Roflumilast
Roflumilast

Theophylline
Theophylline

Tiotropium
Tiotropium

Tulobuterol Hydrochloride
Tulobuterol Hydrochloride

Indacaterol
Indacaterol

Doxofylline
Doxofylline

Indacaterol + Glycopyrronium
Indacaterol + Glycopyrronium