Overview Of Multiple sclerosis
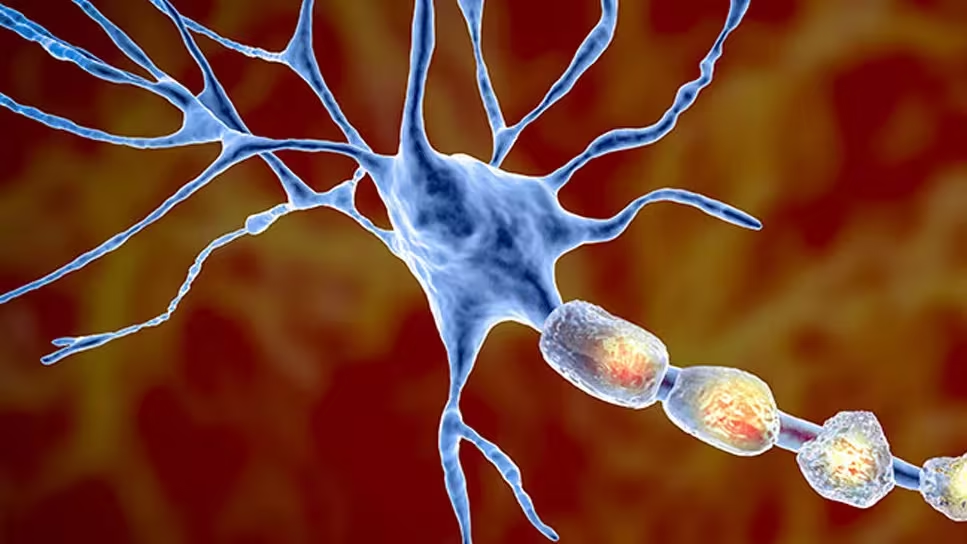
Multiple sclerosis (MS) is a chronic autoimmune disorder of the central nervous system (CNS) characterized by inflammation, demyelination, and neurodegeneration. In MS, the immune system mistakenly attacks the protective myelin sheath surrounding nerve fibers in the brain, spinal cord, and optic nerves, disrupting communication between the brain and the rest of the body. This leads to a wide range of neurological symptoms, including fatigue, muscle weakness, vision problems, and cognitive impairment. MS is classified into several types, including relapsing-remitting MS (RRMS), primary progressive MS (PPMS), and secondary progressive MS (SPMS). The disease typically begins in early adulthood and is more common in women than men. While there is no cure for MS, advancements in treatment have significantly improved disease management and quality of life for patients.
Symptoms of Multiple sclerosis
- The symptoms of multiple sclerosis vary widely depending on the location and extent of nerve damage. Common symptoms include:
- Fatigue: Overwhelming tiredness, often the most debilitating symptom.
- Vision Problems: Blurred vision, double vision, or loss of vision (optic neuritis).
- Muscle Weakness and Spasticity: Stiffness, cramps, or difficulty moving limbs.
- Numbness or Tingling: Often in the face, arms, legs, or trunk.
- Balance and Coordination Issues: Difficulty walking, dizziness, or tremors.
- Cognitive Impairment: Problems with memory, attention, or problem-solving.
- Bladder and Bowel Dysfunction: Urinary urgency, incontinence, or constipation.
- Emotional Changes: Depression, anxiety, or mood swings. Symptoms may come and go (relapses) or worsen progressively over time.
Causes of Multiple sclerosis
- The exact cause of multiple sclerosis remains unknown, but it is believed to result from a combination of genetic, environmental, and immunological factors. Key contributors include:
- Autoimmune Dysfunction: The immune system attacks myelin, leading to inflammation and nerve damage.
- Genetic Predisposition: Family history of MS increases risk, though no single gene is responsible.
- Environmental Factors: - Low vitamin D levels due to limited sunlight exposure. - Smoking, which increases disease severity. - Viral infections, such as Epstein-Barr virus (EBV), which may trigger immune responses.
- Geographic Location: Higher prevalence in temperate climates farther from the equator.
- Age and Gender: Most commonly diagnosed between ages 20-40, with women being 2-3 times more likely to develop MS. Understanding these factors helps in identifying at-risk individuals and developing preventive strategies.
Risk Factors of Multiple sclerosis
- Several factors increase the risk of developing multiple sclerosis:
- Age: Most commonly diagnosed between ages 20-
- Gender: Women are 2-3 times more likely to develop MS than men.
- Family History: Having a close relative with MS increases risk.
- Race: Higher prevalence in Caucasians of Northern European descent.
- Climate: Living in temperate zones farther from the equator.
- Vitamin D Deficiency: Low levels of vitamin D are associated with increased risk.
- Smoking: Smokers are more likely to develop MS and experience faster progression.
- Infections: Previous infections, particularly Epstein-Barr virus (EBV). Identifying these risk factors can help in early detection and intervention.
Prevention of Multiple sclerosis
- While there is no definitive way to prevent multiple sclerosis, certain strategies may reduce the risk or delay disease progression:
- Vitamin D Supplementation: Especially in individuals with low sunlight exposure.
- Smoking Cessation: To reduce disease severity and progression.
- Healthy Lifestyle: Regular exercise, a balanced diet, and stress management.
- Early Treatment: Initiating DMTs at the first sign of MS to slow progression.
- Monitoring for Symptoms: Regular check-ups for individuals with a family history of MS.
- Avoiding Infections: Practicing good hygiene and avoiding known triggers like EBV. By incorporating these strategies, individuals can potentially reduce their risk or improve outcomes.
Prognosis of Multiple sclerosis
- The prognosis for multiple sclerosis varies widely depending on the disease type, severity, and response to treatment. Most individuals with MS have a normal or near-normal life expectancy, though quality of life may be affected by physical and cognitive limitations. Early diagnosis and treatment with DMTs can significantly slow disease progression and reduce relapse rates. However, progressive forms of MS (PPMS, SPMS) may lead to more significant disability over time. Ongoing research and advancements in therapy continue to improve outcomes for individuals with MS.
Complications of Multiple sclerosis
- If left untreated or poorly managed, multiple sclerosis can lead to several complications:
- Severe Disability: Difficulty walking, standing, or performing daily activities.
- Cognitive Decline: Memory loss, difficulty concentrating, or impaired judgment.
- Emotional Disorders: Depression, anxiety, or mood swings.
- Bladder and Bowel Dysfunction: Chronic urinary or fecal incontinence.
- Pressure Sores: Due to immobility or prolonged sitting.
- Osteoporosis: Increased risk of fractures due to reduced mobility.
- Secondary Infections: Such as urinary tract or respiratory infections. Addressing these complications requires a multidisciplinary approach, including medical treatment, therapy, and lifestyle adjustments.
Related Diseases of Multiple sclerosis
- Multiple sclerosis is often associated with other autoimmune or neurological conditions. Related diseases include:
- Neuromyelitis Optica (NMO): A similar condition affecting the optic nerves and spinal cord.
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP): A peripheral nerve disorder.
- Lupus: An autoimmune disease that can affect the nervous system.
- Rheumatoid Arthritis: Another autoimmune condition with overlapping mechanisms.
- Myasthenia Gravis: A neuromuscular disorder causing muscle weakness.
- Fibromyalgia: A condition characterized by chronic pain and fatigue.
- Migraine: Often comorbid with MS due to shared neurological pathways. Understanding these related diseases can help in managing MS more effectively, as they may share common triggers or require similar treatment approaches.
Treatment of Multiple sclerosis
Treatment for multiple sclerosis focuses on managing symptoms, slowing disease progression, and improving quality of life. Common approaches include: 1. **Disease-Modifying Therapies (DMTs)**: - Injectable medications (e.g., interferon beta, glatiramer acetate). - Oral medications (e.g., fingolimod, dimethyl fumarate). - Infusions (e.g., ocrelizumab, natalizumab). 2. **Symptom Management**: - Muscle relaxants (e.g., baclofen) for spasticity. - Antidepressants or antianxiety medications for mood disorders. - Medications for fatigue (e.g., amantadine, modafinil). 3. **Physical Therapy**: To improve mobility, strength, and balance. 4. **Occupational Therapy**: To adapt daily activities and maintain independence. 5. **Lifestyle Modifications**: Regular exercise, a balanced diet, and stress management. 6. **Alternative Therapies**: Acupuncture, yoga, or mindfulness practices. Treatment plans are tailored to the individual’s disease type and symptom severity.
Generics For Multiple sclerosis
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Betamethasone
Betamethasone

Cod Liver Oil (Vitamin A + D)
Cod Liver Oil (Vitamin A + D)

Dexamethasone Sodium Phosphate
Dexamethasone Sodium Phosphate

Lidocaine Hydrochloride + Tolperisone Hydrochloride
Lidocaine Hydrochloride + Tolperisone Hydrochloride

Methylprednisolone Acetate
Methylprednisolone Acetate

Methylprednisolone Sodium Succinate
Methylprednisolone Sodium Succinate

Prednisolone
Prednisolone

Cyclophosphamide
Cyclophosphamide

Interferon Beta 1a
Interferon Beta 1a

Betamethasone
Betamethasone

Cod Liver Oil (Vitamin A + D)
Cod Liver Oil (Vitamin A + D)

Dexamethasone Sodium Phosphate
Dexamethasone Sodium Phosphate

Lidocaine Hydrochloride + Tolperisone Hydrochloride
Lidocaine Hydrochloride + Tolperisone Hydrochloride

Methylprednisolone Acetate
Methylprednisolone Acetate

Methylprednisolone Sodium Succinate
Methylprednisolone Sodium Succinate

Prednisolone
Prednisolone

Cyclophosphamide
Cyclophosphamide

Interferon Beta 1a
Interferon Beta 1a