Overview Of Cystitis
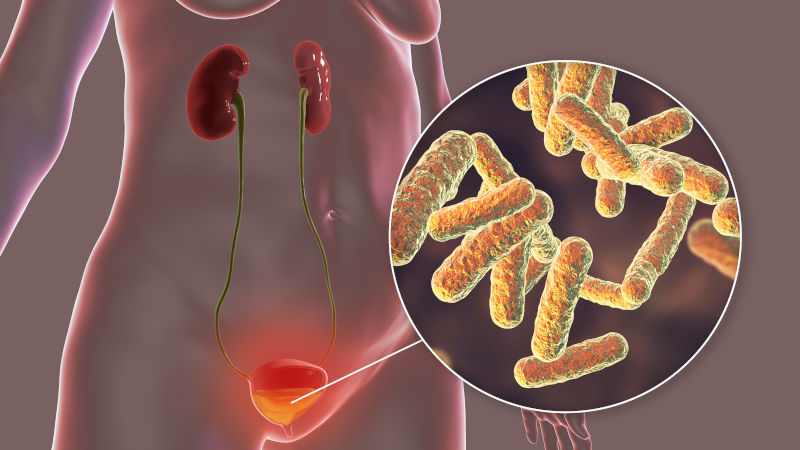
Cystitis is an inflammation of the bladder, most commonly caused by a bacterial infection, although it can also result from non-infectious factors such as chemical irritants, radiation, or autoimmune conditions. It is one of the most common types of urinary tract infections (UTIs) and predominantly affects women due to their shorter urethra, which facilitates bacterial entry into the bladder. Symptoms of cystitis include dysuria (painful urination), frequent urination, urgency, and suprapubic pain. While most cases are mild and resolve with treatment, recurrent or untreated cystitis can lead to complications such as pyelonephritis (kidney infection) or chronic bladder issues. Early diagnosis and appropriate management are essential to prevent complications and improve quality of life.
Symptoms of Cystitis
- The symptoms of cystitis are primarily related to the lower urinary tract and include dysuria (pain or burning during urination), increased urinary frequency, and urgency. Patients may also experience suprapubic pain or pressure and notice cloudy, bloody, or strong-smelling urine. Systemic symptoms such as fever, chills, or flank pain are typically absent in uncomplicated cystitis, as these suggest an upper urinary tract infection (pyelonephritis). In some cases, symptoms may be mild or atypical, particularly in older adults. The onset of symptoms is usually sudden, and their severity can vary depending on the individual and the causative organism.
Causes of Cystitis
- The primary cause of cystitis is bacterial infection, most commonly by *Escherichia coli* (E. coli), which accounts for approximately 75–90% of cases. Other pathogens include *Klebsiella pneumoniae*, *Proteus mirabilis*, and *Staphylococcus saprophyticus*. These bacteria typically originate from the gastrointestinal tract and enter the urinary tract through the urethra. Non-infectious causes of cystitis include chemical irritants (e.g., certain medications, spermicides), radiation therapy, and autoimmune conditions such as interstitial cystitis. Risk factors include sexual activity, use of diaphragms or spermicides, menopause, and urinary tract abnormalities. Poor hygiene practices and delayed urination can also contribute to the development of cystitis.
Risk Factors of Cystitis
- Several factors increase the risk of developing cystitis. Being female is the most significant risk factor due to anatomical differences, such as a shorter urethra and closer proximity to the anus. Sexual activity, particularly with new or multiple partners, can introduce bacteria into the urinary tract. Use of spermicides or diaphragms can alter vaginal flora and increase susceptibility. Postmenopausal women are at higher risk due to decreased estrogen levels, which reduce the protective lactobacilli in the vagina. Other risk factors include a history of previous UTIs, family history, and conditions that impair bladder emptying, such as urinary retention or constipation. Poor hydration and delayed urination can also contribute to the development of cystitis.
Prevention of Cystitis
- Preventing cystitis involves adopting lifestyle and hygiene practices that reduce the risk of bacterial entry into the urinary tract. Increasing fluid intake helps dilute urine and flush out bacteria. Urinating frequently and completely, especially after sexual activity, can prevent bacterial colonization. Proper hygiene, such as wiping from front to back after using the toilet, reduces the risk of introducing bacteria from the anal region to the urethra. Avoiding irritants like spermicides or harsh feminine hygiene products can maintain healthy vaginal flora. For postmenopausal women, topical estrogen therapy may restore protective lactobacilli and reduce UTI risk. In cases of recurrent cystitis, prophylactic antibiotics or postcoital antibiotics may be prescribed under medical supervision.
Prognosis of Cystitis
- The prognosis for cystitis is excellent with appropriate treatment. Most patients experience significant symptom relief within 24–48 hours of starting antibiotics, and the infection is typically fully resolved within a week. Recurrence is common, particularly in women with risk factors such as frequent sexual activity or a history of UTIs. Preventive measures, such as increased hydration, proper hygiene, and postcoital urination, can reduce the likelihood of recurrence. In rare cases, untreated or inadequately treated cystitis can progress to upper urinary tract infections (pyelonephritis) or systemic infections, emphasizing the importance of timely and effective management.
Complications of Cystitis
- While cystitis is generally not life-threatening, it can lead to complications if left untreated or inadequately managed. The most significant complication is the progression to pyelonephritis, an infection of the kidneys that can cause fever, flank pain, and systemic symptoms. Pyelonephritis may lead to sepsis, a life-threatening condition requiring hospitalization and intravenous antibiotics. Recurrent cystitis can cause chronic inflammation and scarring of the bladder, potentially leading to reduced bladder capacity or interstitial cystitis. In pregnant women, untreated cystitis can increase the risk of preterm labor or low birth weight. Rarely, cystitis can result in bacteremia or abscess formation, particularly in immunocompromised individuals.
Related Diseases of Cystitis
- Cystitis is closely associated with several other urinary and reproductive conditions. Recurrent UTIs, defined as three or more infections within a year, are a common related issue, particularly in women. Pyelonephritis, an upper urinary tract infection, can develop if a lower UTI is untreated or spreads to the kidneys. Asymptomatic bacteriuria, the presence of bacteria in the urine without symptoms, is more common in older adults and pregnant women and may require treatment in specific populations. Interstitial cystitis, a chronic bladder condition, can mimic UTI symptoms but is not caused by infection. Sexually transmitted infections (STIs), such as chlamydia or gonorrhea, can present with similar symptoms and should be considered in the differential diagnosis. Understanding these related diseases is essential for accurate diagnosis and comprehensive management.
Treatment of Cystitis
The treatment of cystitis primarily involves a short course of antibiotics, typically lasting 3–7 days. First-line antibiotics include nitrofurantoin, trimethoprim-sulfamethoxazole (TMP-SMX), and fosfomycin. Fluoroquinolones, such as ciprofloxacin, are reserved for cases with resistance to other antibiotics or in patients with allergies. Pain relief can be achieved with phenazopyridine, which alleviates dysuria, but it should not replace antibiotic therapy. Patients are encouraged to increase fluid intake to help flush out bacteria from the urinary tract. Symptoms usually improve within 1–2 days of starting antibiotics, but it is important to complete the full course to prevent recurrence or resistance. Follow-up is generally not required unless symptoms persist or worsen.
Generics For Cystitis
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Aztreonam
Aztreonam

Cefpodoxime
Cefpodoxime

Cefpodoxime + Clavulanic Acid
Cefpodoxime + Clavulanic Acid

Ciprofloxacin
Ciprofloxacin

Flavoxate Hydrochloride
Flavoxate Hydrochloride

Levofloxacin
Levofloxacin

Ofloxacin
Ofloxacin

Pefloxacin
Pefloxacin

Pivmecillinam
Pivmecillinam

Sulphamethoxazole + Trimethoprim (Co-trimoxazole)
Sulphamethoxazole + Trimethoprim (Co-trimoxazole)

Pentosan Polysulphate Sodium
Pentosan Polysulphate Sodium

Aztreonam
Aztreonam

Cefpodoxime
Cefpodoxime

Cefpodoxime + Clavulanic Acid
Cefpodoxime + Clavulanic Acid

Ciprofloxacin
Ciprofloxacin

Flavoxate Hydrochloride
Flavoxate Hydrochloride

Levofloxacin
Levofloxacin

Ofloxacin
Ofloxacin

Pefloxacin
Pefloxacin

Pivmecillinam
Pivmecillinam

Sulphamethoxazole + Trimethoprim (Co-trimoxazole)
Sulphamethoxazole + Trimethoprim (Co-trimoxazole)

Pentosan Polysulphate Sodium
Pentosan Polysulphate Sodium