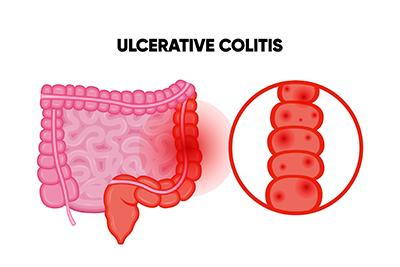
Overview Of Ulcerative colitis
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the colon (large intestine) and rectum. It causes inflammation and the formation of ulcers in the lining of the digestive tract, leading to symptoms like persistent diarrhea, abdominal pain, and rectal bleeding. Unlike other gastrointestinal disorders, ulcerative colitis is a lifelong condition with periods of flare-ups and remission. The severity of the disease varies, with some people experiencing mild symptoms and others suffering from debilitating complications. Though the exact cause is unknown, it is believed to result from an overactive immune response triggered by genetic and environmental factors. Effective management through medication, lifestyle changes, and sometimes surgery can improve quality of life and help achieve long-term remission.
Symptoms of Ulcerative colitis
- Ulcerative colitis presents a wide range of symptoms, which can vary in severity based on the extent of the inflammation:
- Digestive Symptoms: Persistent diarrhea, often accompanied by blood or mucus in the stool, is a hallmark of the disease.
- Abdominal Discomfort: Cramping and pain, especially in the lower abdomen, are common.
- Rectal Issues: Bleeding, urgency to defecate, and a feeling of incomplete evacuation are frequent complaints.
- Systemic Symptoms: Fatigue, weight loss, fever, and reduced appetite often accompany active inflammation.
- Complications of Severe Disease: Severe cases may lead to dehydration, rapid weight loss, and anemia due to blood loss.
Causes of Ulcerative colitis
- The causes of ulcerative colitis are not fully understood, but several factors are believed to contribute to its development:
- Immune System Dysfunction: An abnormal immune response, where the body mistakenly attacks healthy cells in the colon, is a primary suspect.
- Genetic Predisposition: Individuals with a family history of ulcerative colitis or other autoimmune conditions are at higher risk.
- Environmental Triggers: Factors such as diet, air pollution, and exposure to industrial chemicals may exacerbate or trigger symptoms.
- Microbial Imbalance: An imbalance in gut bacteria may disrupt the immune response, causing inflammation.
- Stress and Lifestyle: While not direct causes, stress and poor lifestyle choices can worsen symptoms and trigger flare-ups.
Risk Factors of Ulcerative colitis
- Several factors increase the risk of developing ulcerative colitis:
- Age: Most people are diagnosed between the ages of 15 and 30, with a smaller peak in later adulthood.
- Ethnicity and Geography: Caucasians and people of Ashkenazi Jewish descent are at higher risk, with higher incidence rates in urban areas and developed countries.
- Genetics: Having a close relative, such as a parent or sibling, with ulcerative colitis significantly increases the likelihood of developing the condition.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and a diet high in processed foods may contribute to disease onset or worsen symptoms.
Prevention of Ulcerative colitis
- Although ulcerative colitis cannot be prevented, several strategies can reduce the frequency and severity of flare-ups:
- Medication Adherence: Consistently taking prescribed medications is critical.
- Dietary Adjustments: Avoiding trigger foods, staying hydrated, and consuming anti-inflammatory foods can help.
- Stress Management: Practicing relaxation techniques, like yoga or meditation, can minimize stress-related flare-ups.
- Regular Check-Ups: Monitoring disease progression and addressing issues promptly helps maintain control.
Prognosis of Ulcerative colitis
- The long-term outlook for individuals with ulcerative colitis depends on the severity of the disease and treatment adherence. While there is no cure, proper management can lead to prolonged periods of remission. Advances in medication, including biologics, have significantly improved outcomes for many patients. However, untreated or poorly managed ulcerative colitis can result in serious complications, such as colon cancer, toxic megacolon, or life-threatening bleeding. Regular monitoring and follow-ups with healthcare providers are essential for managing the disease effectively and improving quality of life.
Complications of Ulcerative colitis
- Complications of ulcerative colitis include both short-term and long-term risks:
- Severe Bleeding: Chronic blood loss may lead to anemia.
- Toxic Megacolon: A rare, life-threatening condition where the colon rapidly expands.
- Colon Perforation: Severe inflammation can cause the colon to rupture.
- Cancer Risk: Long-standing ulcerative colitis increases the risk of colorectal cancer.
- Extraintestinal Manifestations: Joint pain, skin disorders, eye inflammation, and liver disease may occur.
Related Diseases of Ulcerative colitis
- Ulcerative colitis is related to several other conditions:
- Crohn’s Disease: Another form of IBD that can affect any part of the digestive tract.
- Irritable Bowel Syndrome (IBS): A functional disorder causing digestive symptoms without inflammation.
- Primary Sclerosing Cholangitis: A liver condition associated with chronic inflammation in the bile ducts.
Treatment of Ulcerative colitis
Treatment for ulcerative colitis aims to reduce inflammation, manage symptoms, and maintain long-term remission: 1. **Medications**: a. Anti-inflammatory drugs, such as aminosalicylates and corticosteroids, are often the first line of treatment. b. Immune suppressors, like azathioprine, cyclosporine, and biologics (infliximab or adalimumab), target the underlying immune response. c. Supportive medications, including antidiarrheal drugs and pain relievers, address specific symptoms. 2. **Lifestyle Modifications**: A balanced diet, stress management techniques, and avoiding trigger foods can reduce flare-ups. 3. **Surgery**: For severe cases or complications, proctocolectomy (removal of the colon and rectum) with an ileal pouch-anal anastomosis or ileostomy may be necessary. Surgery is often curative but requires significant adjustments.
Generics For Ulcerative colitis
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Betamethasone
Betamethasone

Chondroitin + Glucosamine
Chondroitin + Glucosamine

Cyclosporine
Cyclosporine

Dexamethasone Sodium Phosphate
Dexamethasone Sodium Phosphate

Mesalazine
Mesalazine

Methylprednisolone Sodium Succinate
Methylprednisolone Sodium Succinate

Sulfasalazine
Sulfasalazine

Betamethasone
Betamethasone

Chondroitin + Glucosamine
Chondroitin + Glucosamine

Cyclosporine
Cyclosporine

Dexamethasone Sodium Phosphate
Dexamethasone Sodium Phosphate

Mesalazine
Mesalazine

Methylprednisolone Sodium Succinate
Methylprednisolone Sodium Succinate

Sulfasalazine
Sulfasalazine