Overview Of Familial hypercholesterolemia
Familial Hypercholesterolemia (FH) is a genetic disorder characterized by significantly elevated levels of low-density lipoprotein (LDL) cholesterol from birth, leading to an increased risk of premature cardiovascular disease. It is caused by mutations in genes responsible for cholesterol metabolism, such as the LDL receptor gene, apolipoprotein B gene, or PCSK9 gene. These mutations impair the liver's ability to remove LDL cholesterol from the bloodstream, resulting in its accumulation. FH is inherited in an autosomal dominant pattern, meaning only one copy of the defective gene is needed to cause the condition. If left untreated, individuals with FH are at high risk of developing atherosclerosis, heart attacks, and strokes at a young age. Early diagnosis and aggressive treatment are essential to prevent complications.
Symptoms of Familial hypercholesterolemia
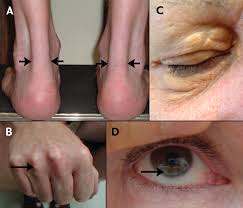
- The symptoms of Familial Hypercholesterolemia are often related to the physical manifestations of high cholesterol and its cardiovascular consequences. Common signs include:
- Xanthomas: Fatty deposits under the skin, particularly on the tendons of the hands, elbows, knees, or Achilles tendons.
- Xanthelasmas: Cholesterol deposits around the eyelids.
- Corneal Arcus: A white or gray ring around the cornea, often seen in younger individuals with FH.
- Chest Pain (Angina): Resulting from reduced blood flow to the heart due to atherosclerosis.
- Heart Attack or Stroke: Premature cardiovascular events, often occurring before the age of 50 in men and 60 in women. Many individuals with FH are asymptomatic until a cardiovascular event occurs, making early screening and diagnosis critical.
Causes of Familial hypercholesterolemia
- Familial Hypercholesterolemia is primarily caused by genetic mutations that disrupt the normal metabolism of LDL cholesterol. The most common mutations occur in:
- LDL Receptor Gene: Mutations here reduce the liver's ability to remove LDL cholesterol from the blood.
- Apolipoprotein B Gene: Mutations affect the binding of LDL particles to their receptors, impairing clearance.
- PCSK9 Gene: Mutations increase the degradation of LDL receptors, reducing their availability. These genetic defects lead to elevated LDL cholesterol levels, even in individuals with a healthy lifestyle. FH is inherited in an autosomal dominant manner, meaning each child of an affected parent has a 50% chance of inheriting the condition. Rarely, FH can result from homozygous mutations, leading to extremely high cholesterol levels and severe cardiovascular disease in childhood.
Risk Factors of Familial hypercholesterolemia
- The primary risk factor for Familial Hypercholesterolemia is a family history of the condition or premature cardiovascular disease. Other risk factors include:
- Genetic Mutations: Inheriting a defective LDL receptor, apolipoprotein B, or PCSK9 gene.
- Age: Cholesterol levels are elevated from birth, increasing the risk of early cardiovascular disease.
- Lifestyle Factors: While FH is genetic, poor diet, lack of exercise, and smoking can exacerbate cholesterol levels and cardiovascular risk.
- Obesity: Excess weight can worsen lipid profiles and increase strain on the cardiovascular system.
- Comorbid Conditions: Diabetes, hypertension, or metabolic syndrome can further elevate cardiovascular risk. Early identification of these risk factors is essential for timely intervention and management.
Prevention of Familial hypercholesterolemia
- While Familial Hypercholesterolemia is a genetic condition and cannot be entirely prevented, early detection and management can mitigate its impact. Key preventive strategies include:
- Genetic Counseling: For families with a history of FH to assess risk and plan for early intervention.
- Cascade Screening: Testing family members of an affected individual to identify and treat FH early.
- Lifestyle Modifications: Adopting a heart-healthy diet, regular exercise, and avoiding smoking.
- Medication Adherence: Taking prescribed medications consistently to control cholesterol levels.
- Regular Monitoring: Frequent lipid testing and cardiovascular assessments to track progress.
- Public Awareness: Educating healthcare providers and the public about FH to promote early diagnosis. By prioritizing these strategies, individuals with FH can reduce their risk of complications and improve their quality of life.
Prognosis of Familial hypercholesterolemia
- The prognosis for individuals with Familial Hypercholesterolemia depends on the severity of the condition, the timeliness of diagnosis, and the effectiveness of treatment. With early and aggressive management, many individuals can achieve near-normal LDL cholesterol levels and significantly reduce their risk of cardiovascular disease. However, untreated or poorly managed FH can lead to premature heart attacks, strokes, and death. Lifelong adherence to treatment and regular follow-up with healthcare providers are critical for maintaining progress and preventing complications. Advances in medications like PCSK9 inhibitors have improved outcomes for many patients with FH.
Complications of Familial hypercholesterolemia
- Untreated Familial Hypercholesterolemia can lead to severe complications, including:
- Atherosclerosis: Accelerated plaque buildup in arteries due to high LDL levels.
- Coronary Artery Disease (CAD): Reduced blood flow to the heart, leading to angina or heart attacks.
- Stroke: Blocked or narrowed arteries in the brain increase stroke risk.
- Peripheral Artery Disease (PAD): Reduced blood flow to the limbs causes pain and increases infection risk.
- Aortic Stenosis: Calcification of the aortic valve due to high cholesterol.
- Premature Death: Cardiovascular events can occur as early as the 30s or 40s without treatment.
- Psychological Impact: The burden of a chronic condition and risk of early death can cause anxiety or depression. Preventing these complications requires lifelong management and adherence to treatment.
Related Diseases of Familial hypercholesterolemia
- Familial Hypercholesterolemia is closely associated with several other conditions, including:
- Atherosclerosis: The primary consequence of high LDL cholesterol, leading to narrowed and hardened arteries.
- Coronary Artery Disease (CAD): A major complication of FH, increasing the risk of heart attacks.
- Stroke: Elevated cholesterol levels contribute to the risk of ischemic stroke.
- Peripheral Artery Disease (PAD): Reduced blood flow to the limbs due to plaque buildup.
- Aortic Stenosis: Calcification of the aortic valve, often seen in individuals with long-standing high cholesterol.
- Metabolic Syndrome: A cluster of conditions, including high blood pressure and insulin resistance, often coexisting with FH.
- Diabetes: Poorly controlled diabetes can exacerbate lipid imbalances in individuals with FH. Understanding these related diseases is essential for comprehensive management and prevention of complications in FH.
Treatment of Familial hypercholesterolemia
Treatment for Familial Hypercholesterolemia focuses on aggressively lowering LDL cholesterol levels to reduce cardiovascular risk. Key strategies include: 1. **Lifestyle Changes**: Adopting a heart-healthy diet (low in saturated fats and cholesterol), regular exercise, and smoking cessation. 2. **Medications**: - **Statins**: First-line therapy to lower LDL cholesterol. - **Ezetimibe**: Reduces cholesterol absorption in the intestines. - **PCSK9 Inhibitors**: Injectable medications that significantly lower LDL levels. - **Bile Acid Sequestrants**: Bind bile acids in the intestines, reducing cholesterol. - **Lomitapide or Mipomersen**: Used in severe cases, particularly homozygous FH. 3. **LDL Apheresis**: A procedure to physically remove LDL cholesterol from the blood for severe or refractory cases. 4. **Regular Monitoring**: Frequent lipid testing to assess treatment efficacy and adjust therapy as needed. A comprehensive treatment plan is essential for managing FH and preventing cardiovascular complications.
Generics For Familial hypercholesterolemia
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Ezetimibe
Ezetimibe

Simvastatin
Simvastatin

Lovastatin
Lovastatin

Fluvastatin
Fluvastatin

Atorvastatin
Atorvastatin

Cholestyramine
Cholestyramine

Rosuvastatin
Rosuvastatin

Ezetimibe
Ezetimibe

Simvastatin
Simvastatin

Lovastatin
Lovastatin

Fluvastatin
Fluvastatin

Atorvastatin
Atorvastatin

Cholestyramine
Cholestyramine

Rosuvastatin
Rosuvastatin