Overview Of Dyslipidemia
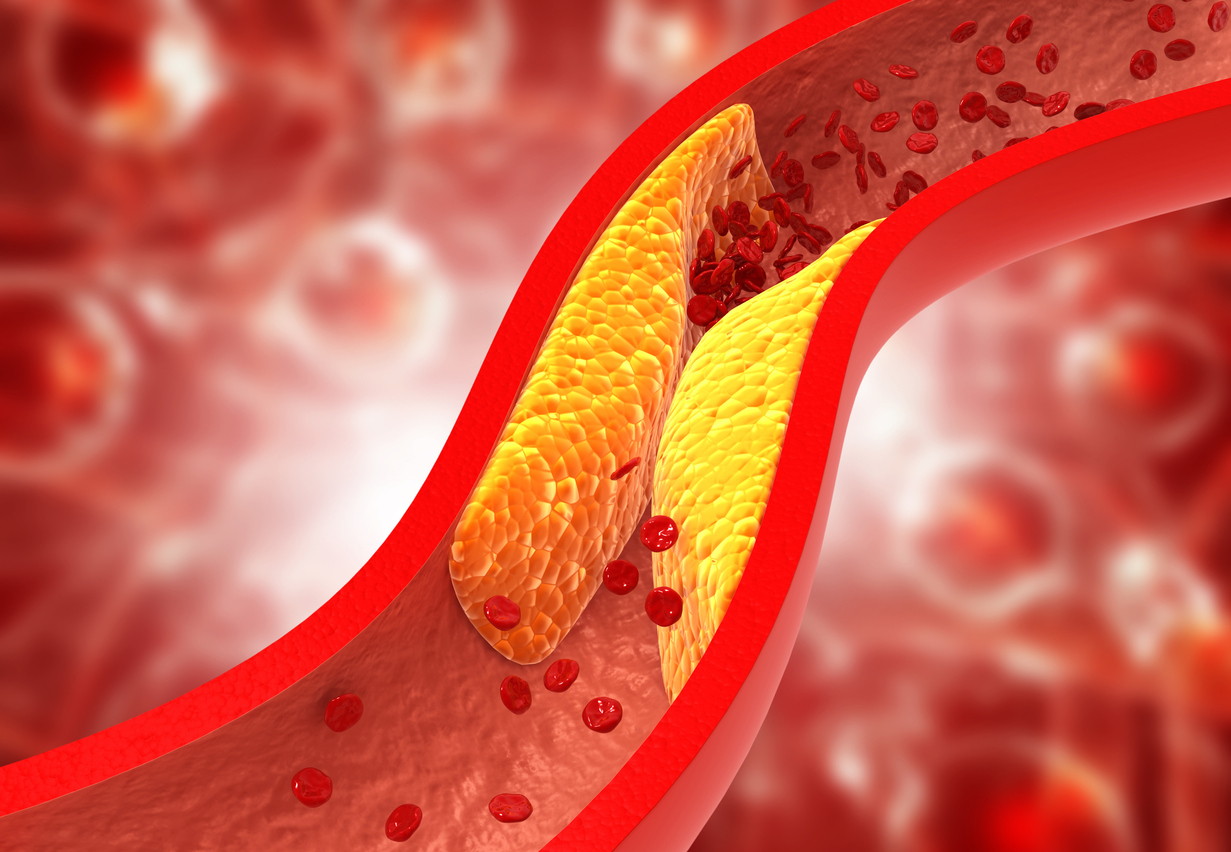
Dyslipidemia is a medical condition characterized by abnormal levels of lipids (fats) in the blood, including elevated cholesterol, triglycerides, or both, as well as low levels of high-density lipoprotein (HDL) cholesterol. Lipids are essential for cellular function, but imbalances can lead to the buildup of plaque in arteries, increasing the risk of cardiovascular diseases such as atherosclerosis, heart attack, and stroke. Dyslipidemia can be primary, resulting from genetic factors, or secondary, caused by lifestyle choices, medical conditions, or medications. Common types include hypercholesterolemia (high LDL cholesterol), hypertriglyceridemia (high triglycerides), and mixed dyslipidemia (elevated LDL and triglycerides with low HDL). Early detection and management are crucial to prevent complications and improve long-term health outcomes.
Symptoms of Dyslipidemia
- Dyslipidemia itself is often asymptomatic, meaning individuals may not experience noticeable symptoms until complications arise. However, severe or prolonged cases can lead to visible signs such as xanthomas (fatty deposits under the skin) or xanthelasmas (cholesterol deposits around the eyelids). In advanced stages, symptoms of cardiovascular disease may develop, including chest pain (angina), shortness of breath, or leg pain during walking (claudication). Acute complications, such as a heart attack or stroke, can present with sudden chest pain, numbness, or difficulty speaking. Routine blood tests are essential for detecting dyslipidemia early, as symptoms often appear only after significant damage has occurred.
Causes of Dyslipidemia
- Dyslipidemia can arise from a combination of genetic, lifestyle, and medical factors. Primary dyslipidemia is often inherited, with conditions like familial hypercholesterolemia causing high cholesterol levels regardless of lifestyle. Secondary dyslipidemia is more common and can result from:
- Unhealthy Diet: High intake of saturated fats, trans fats, and cholesterol.
- Sedentary Lifestyle: Lack of physical activity contributes to weight gain and lipid imbalances.
- Obesity: Excess body fat, particularly abdominal fat, is linked to higher LDL and triglyceride levels.
- Diabetes: Poorly controlled blood sugar levels can disrupt lipid metabolism.
- Hypothyroidism: Low thyroid hormone levels can elevate cholesterol.
- Kidney Disease: Impaired kidney function affects lipid regulation.
- Medications: Drugs like corticosteroids, beta-blockers, and diuretics can alter lipid levels. Understanding these causes helps in tailoring prevention and treatment strategies.
Risk Factors of Dyslipidemia
- Several factors increase the risk of developing dyslipidemia:
- Genetics: Family history of high cholesterol or cardiovascular disease.
- Age and Gender: Lipid levels tend to rise with age, and men are generally at higher risk than premenopausal women.
- Diet: High consumption of saturated fats, trans fats, and cholesterol.
- Physical Inactivity: Lack of exercise contributes to weight gain and poor lipid profiles.
- Obesity: Excess body fat, particularly visceral fat, is strongly linked to dyslipidemia.
- Smoking: Damages blood vessels and lowers HDL cholesterol.
- Chronic Conditions: Diabetes, hypothyroidism, and kidney disease can disrupt lipid metabolism.
- Medications: Certain drugs, such as beta-blockers and diuretics, can alter lipid levels. Addressing these risk factors through lifestyle changes and medical management can reduce the likelihood of developing dyslipidemia.
Prevention of Dyslipidemia
- Preventing dyslipidemia involves adopting a heart-healthy lifestyle and managing risk factors. Key strategies include:
- Healthy Diet: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting saturated fats, trans fats, and cholesterol.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Weight Management: Maintain a healthy weight through balanced nutrition and physical activity.
- Smoking Cessation: Quitting smoking improves HDL cholesterol and overall cardiovascular health.
- Limit Alcohol: Excessive alcohol consumption can raise triglyceride levels.
- Regular Check-ups: Monitor lipid levels and other cardiovascular risk factors through routine blood tests.
- Manage Chronic Conditions: Control diabetes, hypothyroidism, and kidney disease with appropriate medical care. By prioritizing these preventive measures, individuals can significantly reduce their risk of developing dyslipidemia.
Prognosis of Dyslipidemia
- The prognosis for individuals with dyslipidemia depends on the severity of lipid imbalances, the effectiveness of treatment, and the presence of other risk factors. With early diagnosis and appropriate management, many individuals can achieve normal lipid levels and significantly reduce their risk of cardiovascular disease. However, untreated or poorly managed dyslipidemia can lead to serious complications, including heart attack, stroke, and peripheral artery disease. Long-term adherence to lifestyle changes and medications is crucial for maintaining progress and preventing recurrence. Regular follow-up with healthcare providers ensures timely adjustments to treatment plans and ongoing support.
Complications of Dyslipidemia
- Untreated dyslipidemia can lead to several serious complications, including:
- Atherosclerosis: Plaque buildup in arteries narrows blood vessels and restricts blood flow.
- Coronary Artery Disease (CAD): Reduced blood flow to the heart muscle increases the risk of angina and heart attack.
- Stroke: Blocked or narrowed arteries in the brain can cause a stroke.
- Peripheral Artery Disease (PAD): Reduced blood flow to the limbs causes pain and increases the risk of infections.
- Pancreatitis: Extremely high triglyceride levels can trigger inflammation of the pancreas.
- Heart Failure: Chronic strain on the heart from reduced blood flow can lead to heart failure.
- Chronic Kidney Disease: Impaired blood flow to the kidneys can damage their function. Preventing these complications requires diligent management of lipid levels and addressing underlying risk factors.
Related Diseases of Dyslipidemia
- Dyslipidemia is closely associated with several other medical conditions, including:
- Cardiovascular Disease: Atherosclerosis, coronary artery disease, and stroke are direct consequences of untreated dyslipidemia.
- Metabolic Syndrome: A cluster of conditions, including high blood pressure, high blood sugar, and abdominal obesity, often co-occurs with dyslipidemia.
- Diabetes: Poorly controlled blood sugar levels can exacerbate lipid imbalances.
- Hypertension: High blood pressure and dyslipidemia often coexist, increasing cardiovascular risk.
- Chronic Kidney Disease: Impaired kidney function can disrupt lipid metabolism.
- Pancreatitis: Extremely high triglyceride levels can lead to inflammation of the pancreas.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Lipid imbalances contribute to fat accumulation in the liver. Understanding these related diseases is essential for comprehensive management and prevention of dyslipidemia.
Treatment of Dyslipidemia
Treatment for dyslipidemia focuses on lowering LDL cholesterol and triglycerides while raising HDL cholesterol. Strategies include: 1. **Lifestyle Changes**: Adopting a heart-healthy diet (rich in fruits, vegetables, whole grains, and lean proteins), regular exercise, weight management, and smoking cessation. 2. **Medications**: Statins are the first-line treatment for high LDL cholesterol. Other options include ezetimibe, PCSK9 inhibitors, bile acid sequestrants, and fibrates for high triglycerides. 3. **Management of Underlying Conditions**: Controlling diabetes, hypothyroidism, or kidney disease can improve lipid levels. 4. **Regular Monitoring**: Routine blood tests to track lipid levels and adjust treatment as needed. 5. **Therapeutic Lifestyle Changes (TLC)**: A structured program combining diet, exercise, and weight management. A personalized treatment plan is essential for achieving target lipid levels and reducing cardiovascular risk.
Generics For Dyslipidemia
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Fenofibrate
Fenofibrate

Atorvastatin
Atorvastatin

Ezetimibe
Ezetimibe

Fluvastatin
Fluvastatin

Lovastatin
Lovastatin

Niacin (nicotinic acid)
Niacin (nicotinic acid)

Omega-3 fatty acids
Omega-3 fatty acids

Pitavastatin
Pitavastatin

Rosuvastatin
Rosuvastatin

Simvastatin
Simvastatin

Fenofibrate
Fenofibrate

Atorvastatin
Atorvastatin

Ezetimibe
Ezetimibe

Fluvastatin
Fluvastatin

Lovastatin
Lovastatin

Niacin (nicotinic acid)
Niacin (nicotinic acid)

Omega-3 fatty acids
Omega-3 fatty acids

Pitavastatin
Pitavastatin

Rosuvastatin
Rosuvastatin

Simvastatin
Simvastatin