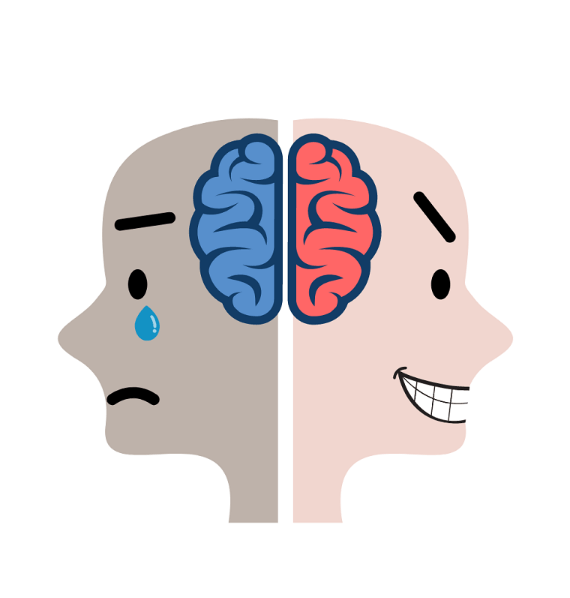
Overview Of Bipolar disorder
Bipolar disorder, formerly known as manic-depressive illness, is a mental health condition characterized by extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). These mood episodes can last for days, weeks, or even months, significantly impacting a person's ability to function in daily life. The disorder is classified into several types, including Bipolar I, Bipolar II, and Cyclothymic Disorder, each varying in the severity and duration of mood episodes. Bipolar I involves at least one manic episode, often accompanied by depressive episodes, while Bipolar II is marked by hypomanic and depressive episodes without full-blown mania. Cyclothymic Disorder involves milder but chronic mood fluctuations. The exact cause of bipolar disorder is not fully understood, but it is believed to result from a combination of genetic, biological, and environmental factors. The condition requires lifelong management, as it can lead to significant impairment in relationships, work, and overall quality of life if left untreated.
Symptoms of Bipolar disorder
- The symptoms of bipolar disorder vary depending on the type and phase of the episode. During manic episodes, individuals may experience elevated mood, increased energy, reduced need for sleep, grandiosity, rapid speech, impulsivity, and risky behaviors such as excessive spending or substance abuse. Hypomanic episodes are similar but less severe and do not typically impair daily functioning. Depressive episodes, on the other hand, are characterized by persistent sadness, loss of interest in activities, fatigue, changes in appetite or weight, sleep disturbances, feelings of worthlessness, difficulty concentrating, and suicidal thoughts. Mixed episodes, which involve symptoms of both mania and depression simultaneously, can be particularly distressing and dangerous. The frequency and intensity of these episodes vary among individuals, with some experiencing rapid cycling (four or more episodes per year). Recognizing these symptoms is crucial for early intervention and effective management of the disorder.
Causes of Bipolar disorder
- The precise causes of bipolar disorder remain unclear, but research suggests a multifaceted interplay of genetic, neurochemical, and environmental factors. Genetically, individuals with a family history of bipolar disorder are at a higher risk, indicating a hereditary component. Neurochemically, imbalances in neurotransmitters such as dopamine, serotonin, and norepinephrine are thought to play a role in mood regulation and the onset of manic or depressive episodes. Structural and functional abnormalities in brain regions responsible for emotional regulation, such as the prefrontal cortex and amygdala, have also been observed in individuals with bipolar disorder. Environmental triggers, such as significant stress, trauma, or substance abuse, can exacerbate or precipitate episodes in genetically predisposed individuals. Additionally, hormonal imbalances and circadian rhythm disruptions may contribute to the disorder's onset. While no single factor is solely responsible, the convergence of these elements creates a predisposition to bipolar disorder.
Risk Factors of Bipolar disorder
- Several risk factors increase the likelihood of developing bipolar disorder. Genetics play a significant role, as having a first-degree relative with the condition substantially elevates risk. Age is another factor, with symptoms typically emerging in late adolescence or early adulthood, although onset can occur at any age. Stressful life events, such as trauma, loss, or major life changes, can trigger episodes in susceptible individuals. Substance abuse, particularly of stimulants or depressants, can exacerbate or mimic symptoms of bipolar disorder. Certain medical conditions, such as thyroid disorders or neurological conditions, may also increase vulnerability. Additionally, gender differences have been observed, with Bipolar I being equally common in men and women, while Bipolar II is more prevalent in women. Understanding these risk factors can aid in early identification and intervention, potentially mitigating the severity of the disorder.
Prevention of Bipolar disorder
- While bipolar disorder cannot be entirely prevented due to its genetic and biological underpinnings, certain strategies can reduce the risk of onset or minimize the severity of episodes. Early intervention is crucial, particularly for individuals with a family history of the disorder or those exhibiting early warning signs such as mood instability or sleep disturbances. Stress management techniques, such as mindfulness, meditation, and regular exercise, can help mitigate triggers. Avoiding substance abuse is essential, as drugs and alcohol can precipitate or worsen episodes. Maintaining a stable lifestyle, including a consistent sleep schedule and balanced diet, can also support mood regulation. For those already diagnosed, adherence to treatment plans, regular follow-up with healthcare providers, and participation in psychotherapy can prevent relapses and promote long-term stability. Educating individuals and their families about the disorder fosters a supportive environment, reducing stigma and encouraging proactive management.
Prognosis of Bipolar disorder
- The prognosis for individuals with bipolar disorder varies widely depending on factors such as the severity of symptoms, adherence to treatment, and the presence of co-occurring conditions. With appropriate and consistent treatment, many individuals can achieve significant symptom reduction and lead fulfilling lives. However, bipolar disorder is a chronic condition that requires lifelong management, and relapses are common, particularly during periods of stress or non-adherence to treatment. Early diagnosis and intervention are associated with better outcomes, as they can prevent the progression of the disorder and reduce the risk of complications such as substance abuse or suicide. Social support, including family involvement and community resources, plays a critical role in improving prognosis. While some individuals may experience residual symptoms or functional impairment, others achieve long-term stability and recovery. Regular follow-up with healthcare providers is essential to monitor progress and adjust treatment as needed.
Complications of Bipolar disorder
- Bipolar disorder can lead to numerous complications if left untreated or poorly managed. One of the most severe risks is suicide, with individuals experiencing depressive episodes being particularly vulnerable. Substance abuse is another common complication, as some may turn to drugs or alcohol to self-medicate or cope with mood swings. The disorder can also strain personal relationships, leading to social isolation or divorce, and impair occupational functioning, resulting in job loss or financial difficulties. Physical health may be affected due to neglect of self-care, poor lifestyle choices, or the side effects of long-term medication use. Additionally, co-occurring psychiatric conditions, such as anxiety disorders or ADHD, can exacerbate symptoms and complicate treatment. Pregnancy and postpartum periods pose unique challenges, as hormonal changes can trigger episodes, and medication use must be carefully managed to ensure the safety of both mother and child. Addressing these complications requires a comprehensive, multidisciplinary approach.
Related Diseases of Bipolar disorder
- Bipolar disorder is often associated with several related psychiatric and medical conditions. Major depressive disorder (MDD) shares overlapping symptoms, particularly during depressive episodes, but lacks the manic or hypomanic phases seen in bipolar disorder. Anxiety disorders, such as generalized anxiety disorder (GAD) or panic disorder, frequently co-occur with bipolar disorder, complicating diagnosis and treatment. Attention-deficit/hyperactivity disorder (ADHD) is another common comorbidity, especially in younger individuals, and can exacerbate impulsivity and mood instability. Substance use disorders are prevalent among those with bipolar disorder, often as a form of self-medication or coping mechanism. Medical conditions such as thyroid disorders, migraines, and cardiovascular disease have also been linked to bipolar disorder, possibly due to shared biological pathways or the side effects of long-term medication use. Recognizing and addressing these related diseases is essential for comprehensive care and improved outcomes.
Treatment of Bipolar disorder
The treatment of bipolar disorder typically involves a combination of pharmacotherapy, psychotherapy, and lifestyle modifications. Mood stabilizers, such as lithium and valproate, are the cornerstone of pharmacological treatment, helping to prevent manic and depressive episodes. Antipsychotics, such as quetiapine or olanzapine, may be used to manage acute symptoms, while antidepressants are sometimes prescribed cautiously for depressive episodes, often in conjunction with mood stabilizers to avoid triggering mania. Psychotherapy, particularly cognitive-behavioral therapy (CBT) and interpersonal and social rhythm therapy (IPSRT), can help individuals manage symptoms, identify triggers, and develop coping strategies. Psychoeducation for patients and their families is also crucial for understanding the disorder and adhering to treatment plans. Lifestyle changes, such as maintaining a regular sleep schedule, avoiding substance abuse, and managing stress, can further support stability. In severe cases, electroconvulsive therapy (ECT) may be considered. Treatment is highly individualized, requiring ongoing adjustments to achieve optimal outcomes.
Generics For Bipolar disorder
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Aripiprazole
Aripiprazole

Carbamazepine
Carbamazepine

Chlorpromazine Hydrochloride
Chlorpromazine Hydrochloride

Citalopram Hydrobromide
Citalopram Hydrobromide

Clonazepam
Clonazepam

Fluoxetine
Fluoxetine

Lamotrigine
Lamotrigine

Olanzapine
Olanzapine

Quetiapine
Quetiapine

Sodium Valproate (valproic acid)
Sodium Valproate (valproic acid)

Ziprasidone
Ziprasidone

Lurasidone
Lurasidone

Aripiprazole
Aripiprazole

Carbamazepine
Carbamazepine

Chlorpromazine Hydrochloride
Chlorpromazine Hydrochloride

Citalopram Hydrobromide
Citalopram Hydrobromide

Clonazepam
Clonazepam

Fluoxetine
Fluoxetine

Lamotrigine
Lamotrigine

Olanzapine
Olanzapine

Quetiapine
Quetiapine

Sodium Valproate (valproic acid)
Sodium Valproate (valproic acid)

Ziprasidone
Ziprasidone

Lurasidone
Lurasidone