Overview Of Epilepsy
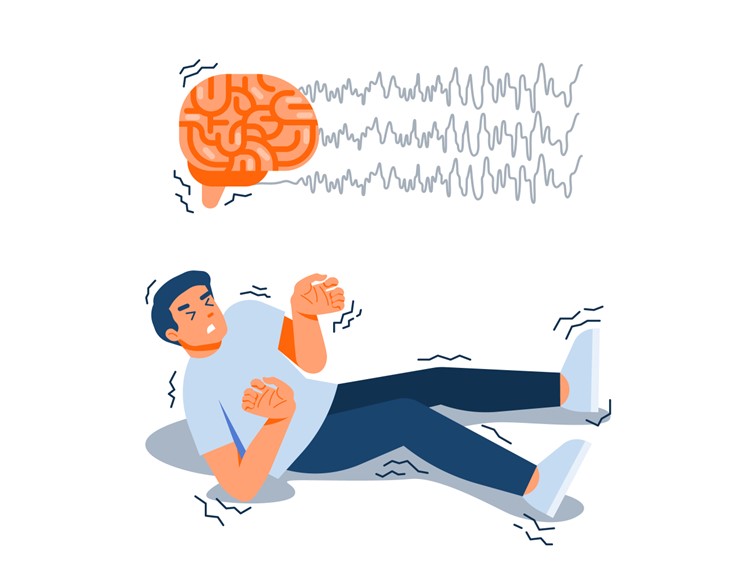
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures. Seizures occur due to sudden, excessive electrical discharges in the brain, which can temporarily disrupt normal brain function. Epilepsy affects people of all ages, genders, and ethnicities, and it is one of the most common neurological conditions worldwide. Seizures can vary widely in their presentation, from brief lapses in awareness to full-body convulsions. Epilepsy is diagnosed when a person experiences two or more unprovoked seizures that are not caused by a temporary underlying condition, such as a high fever or low blood sugar. The condition can have a significant impact on a person’s quality of life, affecting their ability to work, drive, or perform daily activities. However, with proper diagnosis and treatment, many people with epilepsy can lead full and active lives. Epilepsy is a complex condition with various causes, types, and treatment options, making individualized care essential for effective management.
Symptoms of Epilepsy
- The primary symptom of epilepsy is recurrent seizures, which can vary widely in their presentation depending on the part of the brain affected. Focal seizures, which originate in one area of the brain, may cause symptoms such as involuntary movements, sensory changes, or altered emotions without loss of consciousness. Focal seizures with impaired awareness can cause confusion, staring spells, or repetitive movements like lip-smacking or hand-rubbing. Generalized seizures, which involve the entire brain, can cause symptoms such as loss of consciousness, muscle stiffening (tonic seizures), jerking movements (clonic seizures), or sudden loss of muscle tone (atonic seizures). Absence seizures, a type of generalized seizure, are characterized by brief lapses in awareness and staring spells. Some people experience warning signs, known as auras, before a seizure, such as a strange smell, taste, or feeling of déjà vu. Seizures can last from a few seconds to several minutes and may be followed by a period of confusion or fatigue. Recognizing these symptoms is essential for accurate diagnosis and timely intervention.
Causes of Epilepsy
- The causes of epilepsy are diverse and can be broadly categorized into genetic, structural, metabolic, immune, infectious, and unknown causes. Genetic factors play a significant role in some types of epilepsy, with certain genes increasing the likelihood of developing the condition. Structural causes include brain abnormalities present at birth, such as cortical dysplasia, or acquired conditions like traumatic brain injury, stroke, or brain tumors. Metabolic causes involve imbalances in chemicals or nutrients that affect brain function, such as low blood sugar or electrolyte disturbances. Immune-related epilepsy occurs when the immune system mistakenly attacks the brain, leading to inflammation and seizures. Infections, such as meningitis, encephalitis, or neurocysticercosis, can also cause epilepsy by damaging brain tissue. In many cases, the exact cause of epilepsy remains unknown, a condition referred to as idiopathic epilepsy. Understanding the underlying cause is crucial for determining the most effective treatment approach.
Risk Factors of Epilepsy
- Several factors increase the risk of developing epilepsy. Age is a significant risk factor, as epilepsy is more common in children and older adults. A family history of epilepsy or genetic predisposition can increase the likelihood of developing the condition. Brain injuries, such as those caused by trauma, stroke, or infections, are major risk factors for epilepsy. Certain medical conditions, such as Alzheimer’s disease, autism, or cerebral palsy, are also associated with an increased risk of seizures. Prenatal factors, such as maternal infections, poor nutrition, or oxygen deprivation during birth, can contribute to the development of epilepsy in children. Lifestyle factors, such as excessive alcohol consumption or drug use, can increase the risk of seizures. Additionally, individuals with a history of febrile seizures (seizures caused by high fever) during childhood are at higher risk of developing epilepsy later in life. Understanding these risk factors can help identify individuals at higher risk and encourage early intervention.
Prevention of Epilepsy
- While not all cases of epilepsy can be prevented, certain measures can reduce the risk of developing the condition or triggering seizures. Preventing brain injuries by wearing helmets during sports or using seat belts in vehicles can lower the risk of epilepsy caused by trauma. Managing underlying medical conditions, such as diabetes or high blood pressure, can reduce the risk of stroke-related epilepsy. Prenatal care, including proper nutrition and avoiding infections during pregnancy, can help prevent epilepsy in children. For individuals with epilepsy, avoiding known seizure triggers, such as lack of sleep, stress, or flashing lights, can help prevent seizures. Adhering to prescribed medications and treatment plans is essential for maintaining seizure control. Public health initiatives that promote awareness and education about epilepsy can encourage early diagnosis and treatment, improving outcomes for individuals at risk.
Prognosis of Epilepsy
- The prognosis for individuals with epilepsy varies depending on the type and severity of the condition, as well as the effectiveness of treatment. With appropriate treatment, many people with epilepsy can achieve good seizure control and lead full, active lives. However, some individuals may continue to experience seizures despite treatment, a condition known as drug-resistant epilepsy. Early diagnosis and treatment are critical for improving outcomes and preventing complications, such as injuries or cognitive decline. The prognosis is generally better for individuals with idiopathic epilepsy (no identifiable cause) compared to those with structural or metabolic causes. Children with epilepsy often outgrow the condition as they age, particularly if the seizures are well-controlled. Regular follow-up care and adherence to treatment plans are essential for maintaining seizure control and improving quality of life. Advances in treatment options, including new medications and surgical techniques, continue to improve the prognosis for individuals with epilepsy.
Complications of Epilepsy
- Epilepsy can lead to several complications if left untreated or poorly managed. The most immediate risk is injury during a seizure, such as falls, burns, or drowning. Prolonged seizures, known as status epilepticus, are a medical emergency and can cause permanent brain damage or death. Repeated seizures can lead to cognitive decline, memory problems, or learning difficulties, particularly in children. The emotional and psychological impact of epilepsy, including depression, anxiety, and social isolation, can significantly affect quality of life. Sudden unexpected death in epilepsy (SUDEP) is a rare but serious complication that occurs in individuals with poorly controlled seizures. Pregnancy can pose additional risks for women with epilepsy, as seizures and certain medications can affect fetal development. Managing these complications requires a comprehensive approach that includes medical treatment, lifestyle modifications, and mental health support.
Related Diseases of Epilepsy
- Epilepsy is often associated with other neurological and systemic conditions. Migraine, a condition characterized by severe headaches, is more common in individuals with epilepsy. Autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) are also frequently seen in children with epilepsy. Mental health conditions, such as depression and anxiety, are common among individuals with epilepsy due to the emotional and social challenges of living with the condition. Neurodegenerative diseases, such as Alzheimer’s disease, can increase the risk of seizures. Other related conditions include cerebral palsy, intellectual disabilities, and sleep disorders. Understanding these related diseases is essential for providing comprehensive care and improving outcomes for individuals with epilepsy.
Treatment of Epilepsy
The treatment of epilepsy focuses on controlling seizures and improving quality of life. The most common treatment is antiepileptic drugs (AEDs), which help reduce the frequency and severity of seizures. There are many types of AEDs, and the choice of medication depends on the type of seizures, the patient’s age, and potential side effects. In some cases, a combination of medications may be necessary to achieve seizure control. For individuals who do not respond to medication, other treatment options may be considered. Vagus nerve stimulation (VNS) involves implanting a device that sends electrical impulses to the brain to reduce seizures. Responsive neurostimulation (RNS) is another implantable device that monitors brain activity and delivers stimulation to prevent seizures. Surgery may be an option for individuals with focal seizures that originate in a specific area of the brain that can be safely removed. Dietary therapies, such as the ketogenic diet, may be recommended for children or adults with difficult-to-control seizures. A personalized treatment plan, developed in collaboration with a neurologist, is essential for managing epilepsy effectively.
Generics For Epilepsy
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Acetazolamide
Acetazolamide

Allopurinol
Allopurinol

Carbamazepine
Carbamazepine

Clobazam
Clobazam

Clonazepam
Clonazepam

Ethosuximide
Ethosuximide

Flunarizine
Flunarizine

Gabapentin
Gabapentin

Lamotrigine
Lamotrigine

Levetiracetam
Levetiracetam

Oxcarbazepine
Oxcarbazepine

Phenobarbitone (Phenobarbital)
Phenobarbitone (Phenobarbital)

Phenobarbitone Sodium inj
Phenobarbitone Sodium inj

Phenytoin
Phenytoin

Phenytoin Sodium
Phenytoin Sodium

Pregabalin
Pregabalin

Sodium Valproate (valproic acid)
Sodium Valproate (valproic acid)

Thiopental Sodium
Thiopental Sodium

Topiramate
Topiramate

Acetazolamide
Acetazolamide

Allopurinol
Allopurinol

Carbamazepine
Carbamazepine

Clobazam
Clobazam

Clonazepam
Clonazepam

Ethosuximide
Ethosuximide

Flunarizine
Flunarizine

Gabapentin
Gabapentin

Lamotrigine
Lamotrigine

Levetiracetam
Levetiracetam

Oxcarbazepine
Oxcarbazepine

Phenobarbitone (Phenobarbital)
Phenobarbitone (Phenobarbital)

Phenobarbitone Sodium inj
Phenobarbitone Sodium inj

Phenytoin
Phenytoin

Phenytoin Sodium
Phenytoin Sodium

Pregabalin
Pregabalin

Sodium Valproate (valproic acid)
Sodium Valproate (valproic acid)

Thiopental Sodium
Thiopental Sodium

Topiramate
Topiramate