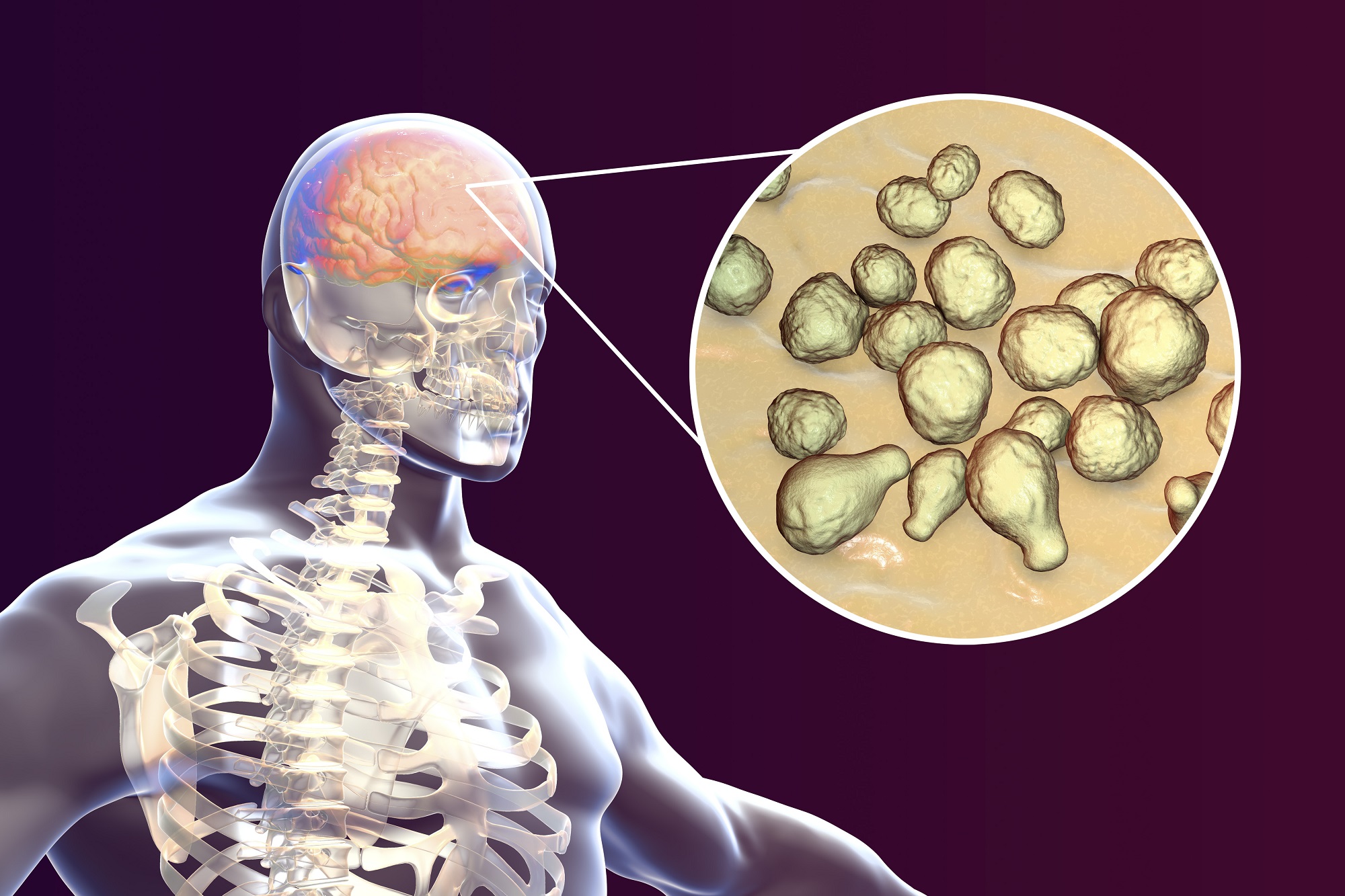
Overview Of Cryptococcal meningitis
Cryptococcal meningitis is a severe fungal infection of the meninges, the protective membranes covering the brain and spinal cord. It is caused by the fungus *Cryptococcus neoformans* or *Cryptococcus gattii*, which are commonly found in soil and bird droppings. The infection primarily affects individuals with weakened immune systems, such as those with HIV/AIDS, organ transplant recipients, or those on immunosuppressive therapies. Symptoms include headache, fever, neck stiffness, nausea, vomiting, confusion, and sensitivity to light. If left untreated, cryptococcal meningitis can lead to permanent neurological damage or death. Early diagnosis and antifungal treatment are essential to improve outcomes and prevent complications.
Symptoms of Cryptococcal meningitis
- The symptoms of cryptococcal meningitis typically develop gradually and may include headache, fever, neck stiffness, nausea, vomiting, confusion, and sensitivity to light (photophobia). As the infection progresses, patients may experience altered mental status, seizures, and focal neurological deficits, such as weakness or vision changes. In immunocompromised individuals, symptoms may be more severe and progress rapidly. Early recognition of symptoms is important for timely diagnosis and treatment, as delayed intervention can lead to severe complications or death.
Causes of Cryptococcal meningitis
- Cryptococcal meningitis is caused by the inhalation of spores from the fungi *Cryptococcus neoformans* or *Cryptococcus gattii*. These fungi are commonly found in soil, decaying wood, and bird droppings. Once inhaled, the spores can disseminate to the central nervous system, particularly in individuals with compromised immune systems. Risk factors include HIV/AIDS, organ transplantation, long-term use of corticosteroids or other immunosuppressive drugs, and chronic diseases such as diabetes or sarcoidosis. Understanding the mode of transmission and risk factors is crucial for prevention and early intervention.
Risk Factors of Cryptococcal meningitis
- Several factors increase the risk of developing cryptococcal meningitis. Immunocompromised individuals, such as those with HIV/AIDS, organ transplant recipients, or those on immunosuppressive therapies, are at the highest risk. Chronic diseases, such as diabetes or sarcoidosis, can also increase susceptibility. Environmental exposure to soil or bird droppings, particularly in endemic regions, further raises the risk. Lack of access to healthcare and delayed diagnosis in resource-limited settings exacerbate the severity of the disease. Addressing these risk factors through preventive measures and early treatment is essential for reducing the incidence of cryptococcal meningitis.
Prevention of Cryptococcal meningitis
- Preventing cryptococcal meningitis involves a combination of medical management, environmental precautions, and public health measures. For high-risk individuals, such as those with HIV/AIDS, prophylactic antifungal therapy with fluconazole may be recommended. Reducing environmental exposure to *Cryptococcus* by avoiding contact with soil or bird droppings, particularly in endemic regions, can lower the risk. Public health initiatives promoting early diagnosis and treatment of HIV/AIDS, as well as access to antifungal medications, play a vital role in reducing the burden of cryptococcal meningitis.
Prognosis of Cryptococcal meningitis
- The prognosis for cryptococcal meningitis depends on the timeliness of diagnosis and treatment, as well as the patient's immune status. With prompt and appropriate antifungal therapy, many patients achieve significant improvement and recovery. However, the mortality rate remains high, particularly in resource-limited settings or in patients with advanced HIV/AIDS. Long-term complications, such as neurological deficits or recurrent infections, may occur in some cases. Early diagnosis, adherence to treatment, and follow-up care are essential for improving prognosis and preventing long-term complications.
Complications of Cryptococcal meningitis
- If left untreated or inadequately managed, cryptococcal meningitis can lead to severe complications. Increased intracranial pressure can cause brain herniation, a life-threatening condition. Permanent neurological damage, such as cognitive impairment, vision loss, or hearing loss, may occur due to inflammation and tissue damage. Recurrent infections are common in immunocompromised individuals, particularly if antifungal therapy is not continued long-term. Early diagnosis and treatment are crucial to minimize the risk of these complications.
Related Diseases of Cryptococcal meningitis
- Cryptococcal meningitis is closely related to other fungal infections caused by *Cryptococcus* species, such as pulmonary cryptococcosis, which affects the lungs. It is also associated with conditions that compromise the immune system, such as HIV/AIDS, organ transplantation, and chronic diseases like diabetes or sarcoidosis. Other related conditions include other forms of meningitis, such as bacterial or viral meningitis, which share similar symptoms but have different causative agents and treatment approaches. Understanding these relationships is essential for accurate diagnosis, effective treatment, and comprehensive prevention of central nervous system infections.
Treatment of Cryptococcal meningitis
The treatment of cryptococcal meningitis involves a combination of antifungal medications and supportive care. The initial phase of treatment typically includes intravenous amphotericin B and flucytosine for at least 2 weeks, followed by oral fluconazole for several months to prevent relapse. In resource-limited settings, fluconazole may be used as monotherapy, although it is less effective. Supportive care, including management of increased intracranial pressure, seizures, and secondary infections, is essential. Early and aggressive treatment is crucial to improve outcomes and prevent complications.
Generics For Cryptococcal meningitis
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Amphotericin B
Amphotericin B

Fluconazole
Fluconazole

Fluconazole 0.2% IV
Fluconazole 0.2% IV

Itraconazole
Itraconazole

Amphotericin B
Amphotericin B

Fluconazole
Fluconazole

Fluconazole 0.2% IV
Fluconazole 0.2% IV

Itraconazole
Itraconazole