Overview Of Crohn's disease
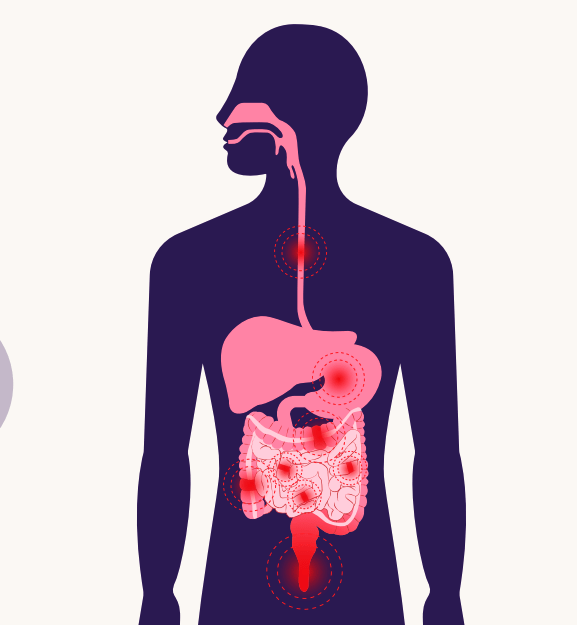
Crohn's disease is a type of inflammatory bowel disease (IBD) that causes chronic inflammation of the gastrointestinal (GI) tract. It can affect any part of the GI tract, from the mouth to the anus, but most commonly involves the end of the small intestine (ileum) and the beginning of the colon. Crohn's disease is characterized by periods of flare-ups (active symptoms) and remission (no symptoms). The inflammation caused by Crohn's disease often spreads deep into the layers of affected bowel tissue, leading to complications such as strictures, fistulas, and malnutrition. It is a lifelong condition with no known cure, but treatments can help manage symptoms and improve quality of life.
Symptoms of Crohn's disease
- The symptoms of Crohn's disease vary depending on the location and severity of inflammation. Common symptoms include: Digestive Issues: Persistent diarrhea, abdominal pain, and cramping. Weight Loss: Unintentional weight loss due to malabsorption of nutrients. Fatigue: Chronic tiredness caused by inflammation and anemia. Fever: Low-grade fever during flare-ups. Rectal Bleeding: Blood in the stool due to ulcers or fissures. Reduced Appetite: Loss of appetite and nausea. Perianal Symptoms: Pain, drainage, or swelling near the anus due to fistulas or abscesses. Extraintestinal symptoms may also occur, including joint pain, skin rashes, and eye inflammation.
Causes of Crohn's disease
- The exact cause of Crohn's disease is unknown, but it is believed to result from a combination of factors: Immune System Dysfunction: An abnormal immune response may cause the immune system to attack the GI tract, leading to inflammation. Genetics: A family history of Crohn's disease increases the risk, suggesting a genetic predisposition. Environmental Factors: Factors such as diet, smoking, and exposure to certain microbes may trigger or worsen the disease. Gut Microbiome Imbalance: Disruptions in the balance of gut bacteria may contribute to inflammation. Autoimmune Component: The immune system may mistakenly target healthy cells in the digestive tract.
Risk Factors of Crohn's disease
- Several factors increase the risk of developing Crohn's disease: Age: Most commonly diagnosed in individuals between 15 and 35, though it can occur at any age. Family History: Having a close relative with Crohn's disease increases the risk. Smoking: Smokers are at higher risk and tend to have more severe symptoms. Ethnicity: More common in people of Ashkenazi Jewish descent. Geographic Location: Higher prevalence in urban areas and industrialized countries. Medications: Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) may increase risk.
Prevention of Crohn's disease
- While Crohn's disease cannot be entirely prevented, certain measures may reduce the risk or severity of flare-ups: Healthy Diet: Avoiding trigger foods and maintaining a balanced diet. Smoking Cessation: Quitting smoking to reduce disease severity. Stress Management: Techniques such as yoga, meditation, or counseling to manage stress. Regular Monitoring: Routine check-ups and adherence to treatment plans. Exercise: Regular physical activity to support overall health.
Prognosis of Crohn's disease
- The prognosis for Crohn's disease varies depending on the severity and response to treatment. While there is no cure, many patients achieve long-term remission with proper management. However, the disease often involves recurrent flare-ups, and complications may arise over time. Early diagnosis and adherence to treatment plans can significantly improve outcomes and quality of life.
Complications of Crohn's disease
- Crohn's disease can lead to serious complications if not managed effectively: Bowel Obstruction: Scarring and narrowing of the intestine can block the passage of stool. Fistulas: Abnormal connections between the intestine and other organs or skin. Abscesses: Pockets of infection in the abdomen or around the anus. Ulcers: Open sores in the digestive tract. Malnutrition: Poor absorption of nutrients due to inflammation. Colon Cancer: Increased risk of colon cancer with long-standing Crohn's disease. Osteoporosis: Weakened bones due to malabsorption of calcium and vitamin D.
Related Diseases of Crohn's disease
- Crohn's disease is often associated with other conditions, including: Ulcerative Colitis: Another type of inflammatory bowel disease that affects the colon. Irritable Bowel Syndrome (IBS): A functional GI disorder with overlapping symptoms. Celiac Disease: An autoimmune reaction to gluten that damages the small intestine. Arthritis: Joint inflammation commonly seen in IBD patients. Skin Disorders: Conditions like erythema nodosum or pyoderma gangrenosum. Liver Disease: Primary sclerosing cholangitis (PSC) is associated with Crohn's disease.
Treatment of Crohn's disease
Treatment for Crohn's disease aims to reduce inflammation, manage symptoms, and prevent complications. Options include: Medications: Anti-inflammatory drugs (e.g., corticosteroids, aminosalicylates). Immune system suppressors (e.g., azathioprine, methotrexate). Biologics (e.g., infliximab, adalimumab) to target specific immune responses. Antibiotics to treat infections or fistulas. Antidiarrheal and pain relievers for symptom management. Nutrition Therapy: Special diets or enteral nutrition to reduce inflammation and improve nutrition. Surgery: Required for complications such as strictures, fistulas, or abscesses. Common procedures include bowel resection or strictureplasty. Immune System Suppressors: Medications like azathioprine or methotrexate to suppress the immune response. Biologics: Targeted therapies that neutralize specific proteins involved in inflammation, such as TNF inhibitors. Antibiotics: To treat or prevent infections, especially in cases of fistulas or abscesses. Diet and Nutrition Therapy: Special diets or nutritional supplements to manage symptoms and address deficiencies. Surgery: Removing damaged portions of the digestive tract when other treatments are ineffective. Lifestyle and Home Remedies: Stress management, regular exercise, and smoking cessation to help manage symptoms.
Generics For Crohn's disease
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Ciprofloxacin
Ciprofloxacin

Loperamide
Loperamide

Mercaptopurine
Mercaptopurine

Metronidazole
Metronidazole

Propantheline Bromide
Propantheline Bromide

Sulfasalazine
Sulfasalazine

Azathioprine
Azathioprine

Methotrexate
Methotrexate

Cholestyramine
Cholestyramine

Acarbose
Acarbose

Ciprofloxacin
Ciprofloxacin

Loperamide
Loperamide

Mercaptopurine
Mercaptopurine

Metronidazole
Metronidazole

Propantheline Bromide
Propantheline Bromide

Sulfasalazine
Sulfasalazine

Azathioprine
Azathioprine

Methotrexate
Methotrexate

Cholestyramine
Cholestyramine

Acarbose
Acarbose