Overview Of Hyperlipidaemia
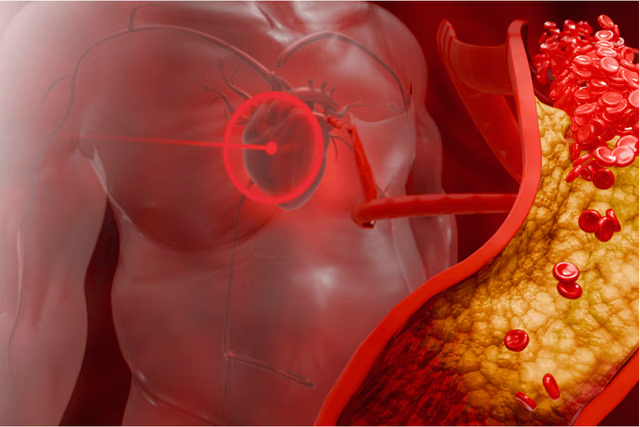
Hyperlipidaemia is a medical condition characterized by abnormally high levels of lipids (fats) in the blood, including cholesterol and triglycerides. These lipids are essential for normal body function, but excessive amounts can lead to the buildup of plaque in the arteries, a condition known as atherosclerosis. This plaque narrows and hardens the arteries, restricting blood flow and increasing the risk of cardiovascular diseases such as heart attacks and strokes. Hyperlipidaemia is often categorized into two main types: hypercholesterolaemia (high cholesterol) and hypertriglyceridaemia (high triglycerides). It can be primary, caused by genetic factors, or secondary, resulting from lifestyle choices or other medical conditions. The condition is often asymptomatic, meaning individuals may not realize they have it until they experience a serious cardiovascular event. Early detection and management are crucial to prevent complications and improve long-term health outcomes. ---
Symptoms of Hyperlipidaemia
- Hyperlipidaemia is often referred to as a "silent" condition because it typically does not cause noticeable symptoms until it leads to serious complications such as atherosclerosis, heart attack, or stroke. However, in rare cases, extremely high levels of triglycerides can cause symptoms like abdominal pain, pancreatitis, or xanthomas (fatty deposits under the skin). High cholesterol levels may also lead to the development of xanthelasmas (yellowish patches around the eyes) or arcus corneae (a white or gray ring around the cornea of the eye). These physical signs are more common in individuals with genetic forms of hyperlipidaemia. For most people, the condition is detected through routine blood tests that measure lipid levels. Regular screening is essential, especially for those with risk factors such as a family history of heart disease, obesity, or diabetes. ---
Causes of Hyperlipidaemia
- Hyperlipidaemia can be caused by a combination of genetic, lifestyle, and medical factors. Primary hyperlipidaemia is often inherited, with conditions such as familial hypercholesterolaemia leading to excessively high cholesterol levels regardless of lifestyle. Secondary hyperlipidaemia is more common and is influenced by modifiable factors such as a diet high in saturated fats, trans fats, and cholesterol, as well as physical inactivity and obesity. Medical conditions like diabetes, hypothyroidism, kidney disease, and liver disease can also contribute to elevated lipid levels. Certain medications, including corticosteroids, beta-blockers, and diuretics, may exacerbate the condition. Additionally, excessive alcohol consumption and smoking are significant risk factors. Understanding the underlying cause is essential for tailoring effective treatment strategies and reducing the risk of cardiovascular complications. ---
Risk Factors of Hyperlipidaemia
- Several risk factors contribute to the development of hyperlipidaemia, many of which are modifiable through lifestyle changes or medical interventions. Key modifiable risk factors include a diet high in saturated fats, trans fats, and cholesterol, as well as physical inactivity and obesity. Non-modifiable risk factors include age (lipid levels tend to increase with age), gender (men are generally at higher risk, though women's risk increases after menopause), and a family history of hyperlipidaemia or cardiovascular disease. Other contributing factors include medical conditions such as diabetes, hypothyroidism, and chronic kidney disease, as well as certain medications like corticosteroids and beta-blockers. Lifestyle factors such as smoking and excessive alcohol consumption also play a significant role. Addressing these risk factors through lifestyle modifications and medical management is crucial for reducing the risk of hyperlipidaemia and its complications. ---
Prevention of Hyperlipidaemia
- Preventing hyperlipidaemia involves addressing modifiable risk factors through lifestyle changes and medical interventions. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins, while limiting saturated fats, trans fats, and cholesterol, is essential. Regular physical activity, such as brisk walking or cycling, helps maintain a healthy weight and improves lipid levels. Smoking cessation and limiting alcohol consumption are also critical. Managing underlying medical conditions such as diabetes, hypothyroidism, and high blood pressure is important for preventing secondary hyperlipidaemia. Regular health check-ups and lipid screenings enable early detection and intervention, significantly lowering the likelihood of developing hyperlipidaemia and its complications. Public health initiatives promoting healthy lifestyles and awareness of cardiovascular risk factors also play a vital role in prevention. ---
Prognosis of Hyperlipidaemia
- The prognosis for individuals with hyperlipidaemia is generally favorable with appropriate management and adherence to treatment plans. Lifestyle modifications and medications can significantly reduce lipid levels and lower the risk of cardiovascular complications such as heart attack and stroke. However, the condition requires ongoing monitoring and management, as it is often chronic and influenced by factors such as diet, physical activity, and underlying medical conditions. Regular follow-up with a healthcare provider, adherence to prescribed medications, and consistent lifestyle changes are critical for maintaining a positive prognosis. Early diagnosis and intervention are key to preventing long-term complications and ensuring the best possible outcomes for patients. ---
Complications of Hyperlipidaemia
- If left untreated or poorly managed, hyperlipidaemia can lead to serious complications, primarily related to the cardiovascular system. The most significant risk is the development of atherosclerosis, where plaque buildup narrows and hardens the arteries, restricting blood flow. This can result in coronary artery disease, heart attack, stroke, or peripheral artery disease. High triglyceride levels can also lead to pancreatitis, a painful and potentially life-threatening inflammation of the pancreas. Additionally, hyperlipidaemia is often associated with other metabolic conditions such as diabetes and metabolic syndrome, further increasing the risk of cardiovascular complications. Early diagnosis and effective management are crucial to minimizing the risk of these complications and ensuring the best possible outcomes for patients. ---
Related Diseases of Hyperlipidaemia
- Hyperlipidaemia is closely related to several other medical conditions, particularly those involving the cardiovascular system. These include atherosclerosis, coronary artery disease, heart attack, and stroke, all of which result from the buildup of plaque in the arteries. Peripheral artery disease (PAD), characterized by narrowed arteries in the limbs, is also associated with hyperlipidaemia. Additionally, the condition is often linked to metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and diabetes. Other related conditions include pancreatitis, which can result from extremely high triglyceride levels, and non-alcoholic fatty liver disease (NAFLD), which is associated with abnormal lipid metabolism. Understanding these relationships is essential for comprehensive management and prevention of hyperlipidaemia and its complications. ---
Treatment of Hyperlipidaemia
The treatment of hyperlipidaemia focuses on reducing lipid levels to lower the risk of cardiovascular disease. The first line of treatment typically involves lifestyle modifications, such as adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins while limiting saturated fats, trans fats, and cholesterol. Regular physical activity, weight management, and smoking cessation are also crucial. Medications are often prescribed for individuals who do not achieve target lipid levels through lifestyle changes alone. Common medications include statins, which lower LDL cholesterol; fibrates, which reduce triglycerides; and niacin, which can improve both cholesterol and triglyceride levels. Other options include bile acid sequestrants, cholesterol absorption inhibitors, and PCSK9 inhibitors. Treatment plans are tailored to the individual's specific lipid profile, risk factors, and overall health status. ---
Generics For Hyperlipidaemia
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Amlodipine 5mg + Atorvastatin 10mg
Amlodipine 5mg + Atorvastatin 10mg

Ezetimibe
Ezetimibe

Fenofibrate
Fenofibrate

Inositol nicotinate
Inositol nicotinate

Lovastatin
Lovastatin

Niacin (nicotinic acid)
Niacin (nicotinic acid)

Rosuvastatin
Rosuvastatin

Salmon Oil
Salmon Oil

Simvastatin
Simvastatin

Fluvastatin
Fluvastatin

Cholestyramine
Cholestyramine

Amlodipine 5mg + Atorvastatin 10mg
Amlodipine 5mg + Atorvastatin 10mg

Ezetimibe
Ezetimibe

Fenofibrate
Fenofibrate

Inositol nicotinate
Inositol nicotinate

Lovastatin
Lovastatin

Niacin (nicotinic acid)
Niacin (nicotinic acid)

Rosuvastatin
Rosuvastatin

Salmon Oil
Salmon Oil

Simvastatin
Simvastatin

Fluvastatin
Fluvastatin

Cholestyramine
Cholestyramine