Overview Of Osteoarthritis & degenerative arthritis
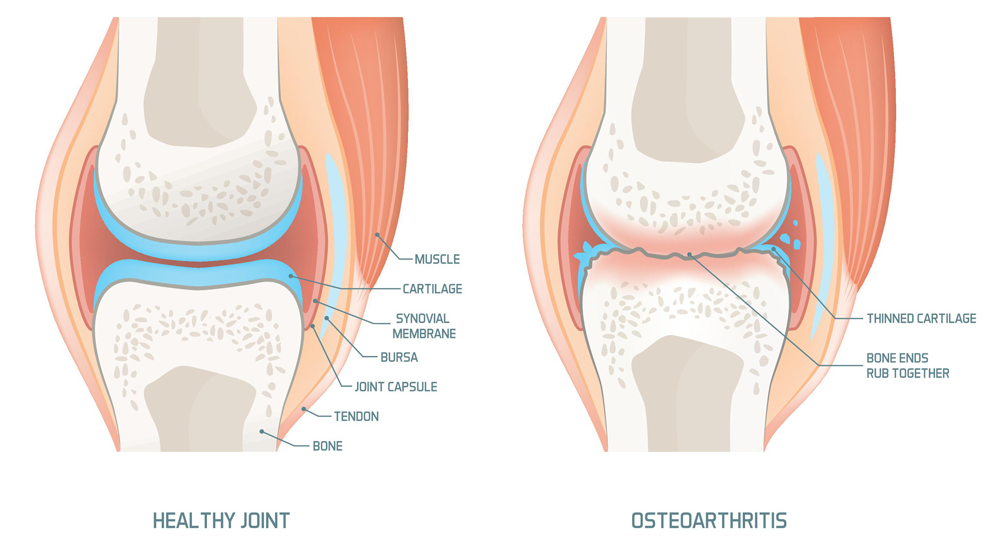
Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide. It is a degenerative joint disease characterized by the breakdown of cartilage, the flexible tissue that cushions the ends of bones in joints. As cartilage wears down, bones begin to rub against each other, causing pain, swelling, and stiffness. Osteoarthritis most commonly affects weight-bearing joints such as the knees, hips, and spine, but it can also occur in the hands, fingers, and other joints. The condition typically develops gradually over time, and its severity can range from mild discomfort to debilitating pain and loss of mobility. While osteoarthritis is often associated with aging, it is not an inevitable part of getting older. Factors such as joint injury, obesity, genetics, and overuse of joints can contribute to its development. Osteoarthritis is a leading cause of disability, particularly among older adults, and can significantly impact quality of life. However, with proper management, including lifestyle changes, medications, and therapies, many people with osteoarthritis can maintain an active and fulfilling life. Early diagnosis and intervention are key to slowing the progression of the disease and minimizing its impact.
Symptoms of Osteoarthritis & degenerative arthritis
- The symptoms of osteoarthritis vary depending on the affected joint and the severity of the condition. Common symptoms include joint pain, which is often described as a deep, aching sensation that worsens with activity and improves with rest. Stiffness, particularly in the morning or after periods of inactivity, is another hallmark symptom. Swelling around the joint may occur due to inflammation or the formation of bone spurs. Reduced range of motion and flexibility can make it difficult to perform everyday tasks, such as bending, climbing stairs, or gripping objects. In some cases, joints may produce a grating or cracking sound, known as crepitus, during movement. Osteoarthritis in the hands can lead to the development of bony nodules, such as Heberden’s nodes at the fingertips or Bouchard’s nodes in the middle joints. As the condition progresses, joint deformities and instability may occur, further limiting mobility and increasing pain. Symptoms can fluctuate, with periods of relative relief followed by flare-ups of increased pain and inflammation. Early recognition of these symptoms is crucial for timely diagnosis and management.
Causes of Osteoarthritis & degenerative arthritis
- Osteoarthritis is primarily caused by the gradual breakdown of cartilage in the joints, but the exact cause is often multifactorial. Aging is one of the most significant risk factors, as cartilage naturally becomes less resilient and more prone to damage over time. Joint injuries, such as those sustained during sports or accidents, can also lead to osteoarthritis, even years after the injury has healed. Repetitive stress on joints from certain occupations or activities can accelerate cartilage wear and tear. Obesity is another major contributor, as excess weight places additional stress on weight-bearing joints like the knees and hips. Genetics play a role, as some people inherit a predisposition to developing osteoarthritis. Other factors include bone deformities, such as misaligned joints, and certain metabolic disorders that affect cartilage health. Inflammatory conditions, such as rheumatoid arthritis, can also increase the risk of developing osteoarthritis. While the exact mechanisms are not fully understood, it is clear that a combination of mechanical, genetic, and environmental factors contribute to the onset and progression of osteoarthritis.
Risk Factors of Osteoarthritis & degenerative arthritis
- Several factors increase the risk of developing osteoarthritis. Age is the most significant risk factor, as cartilage naturally deteriorates over time. Joint injuries, such as fractures, ligament tears, or dislocations, can predispose individuals to osteoarthritis, even if the injury occurred years earlier. Repetitive stress on joints from occupations or activities that involve kneeling, lifting, or repetitive motions can accelerate cartilage wear. Obesity is a major risk factor, as excess weight places additional stress on weight-bearing joints like the knees and hips. Genetics also play a role, with certain inherited traits increasing susceptibility to cartilage damage. Bone deformities, such as misaligned joints or unequal leg length, can contribute to uneven wear and tear on joints. Gender is another factor, as women are more likely than men to develop osteoarthritis, particularly after menopause. Other medical conditions, such as diabetes, gout, or rheumatoid arthritis, can increase the risk. Understanding these risk factors can help individuals take preventive measures and seek early intervention if symptoms arise.
Prevention of Osteoarthritis & degenerative arthritis
- Preventing osteoarthritis involves a combination of lifestyle modifications and proactive measures to protect joint health. Maintaining a healthy weight is one of the most effective ways to reduce stress on weight-bearing joints like the knees and hips. Regular exercise, particularly low-impact activities such as swimming or cycling, can strengthen the muscles around joints and improve flexibility. Avoiding repetitive stress on joints and using proper techniques during physical activities can help prevent injuries that may lead to osteoarthritis. Wearing supportive footwear and using ergonomic tools can also reduce joint strain. For individuals with a family history of osteoarthritis or other risk factors, early intervention and regular monitoring can help detect and manage the condition before it progresses. A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, may also support joint health. Public health initiatives that promote awareness and education about osteoarthritis prevention are essential for reducing the burden of this condition.
Prognosis of Osteoarthritis & degenerative arthritis
- The prognosis for individuals with osteoarthritis varies depending on the severity of the condition, the affected joints, and the effectiveness of treatment. While osteoarthritis is a chronic and progressive disease, many people can manage their symptoms and maintain a good quality of life with appropriate care. Early diagnosis and intervention are critical for slowing the progression of joint damage and minimizing pain. Weight management, regular exercise, and adherence to treatment plans can significantly improve outcomes. However, in some cases, osteoarthritis can lead to significant disability, particularly if it affects weight-bearing joints like the knees or hips. Surgical interventions, such as joint replacement, can provide long-term relief for severe cases. The emotional and psychological impact of osteoarthritis, including depression and anxiety, should not be overlooked, as these can affect overall well-being and adherence to treatment. With ongoing research and advances in treatment options, the prognosis for individuals with osteoarthritis continues to improve.
Complications of Osteoarthritis & degenerative arthritis
- Osteoarthritis can lead to several complications if left untreated or poorly managed. Chronic pain and stiffness can significantly impact mobility and quality of life, making it difficult to perform daily activities. Over time, joint deformities and instability may develop, increasing the risk of falls and injuries. In severe cases, osteoarthritis can lead to complete loss of cartilage, resulting in bone-on-bone contact and severe pain. This can necessitate surgical interventions, such as joint replacement. Osteoarthritis in the spine can cause nerve compression, leading to symptoms such as numbness, tingling, or weakness in the limbs. The emotional and psychological impact of living with chronic pain and disability can also lead to depression, anxiety, and social isolation. Additionally, the use of long-term pain medications, such as NSAIDs, can have side effects, including gastrointestinal bleeding or kidney damage. Addressing these complications requires a comprehensive approach that includes medical treatment, physical therapy, and mental health support.
Related Diseases of Osteoarthritis & degenerative arthritis
- Osteoarthritis is often associated with other joint and musculoskeletal conditions. Rheumatoid arthritis, an autoimmune disorder that causes inflammation in the joints, can coexist with osteoarthritis and complicate its management. Gout, a form of arthritis caused by the buildup of uric acid crystals in the joints, can also occur alongside osteoarthritis. Osteoporosis, a condition characterized by weakened bones, is more common in individuals with osteoarthritis, particularly in older adults. Fibromyalgia, a chronic pain disorder, can exacerbate the symptoms of osteoarthritis and make diagnosis and treatment more challenging. Other related conditions include bursitis, tendonitis, and spinal stenosis, which can cause similar symptoms and require differentiated diagnosis. Understanding these related diseases is essential for providing comprehensive care and improving outcomes for individuals with osteoarthritis.
Treatment of Osteoarthritis & degenerative arthritis
The treatment of osteoarthritis focuses on relieving symptoms, improving joint function, and slowing the progression of the disease. Non-pharmacological approaches are often the first line of treatment and include weight management, physical therapy, and exercise. Weight loss can significantly reduce stress on weight-bearing joints, while physical therapy can improve strength, flexibility, and range of motion. Low-impact exercises, such as swimming or cycling, are particularly beneficial. Medications, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), are commonly used to manage pain and inflammation. Topical creams or gels containing NSAIDs or capsaicin can provide localized relief. For more severe pain, corticosteroid injections or hyaluronic acid injections may be recommended. In cases where conservative treatments are ineffective, surgical options, such as joint replacement or arthroscopy, may be considered. Assistive devices, such as braces, canes, or shoe inserts, can help reduce joint stress and improve mobility. Lifestyle modifications, such as avoiding activities that exacerbate symptoms and using ergonomic tools, can also play a key role in managing osteoarthritis. A personalized treatment plan, developed in collaboration with a healthcare provider, is essential for achieving the best outcomes.
Generics For Osteoarthritis & degenerative arthritis
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Aceclofenac
Aceclofenac

Acemetacin
Acemetacin

Capsaicin 0.025% topical
Capsaicin 0.025% topical

Celecoxib
Celecoxib

Chondroitin + Glucosamine
Chondroitin + Glucosamine

Cod Liver Oil (Vitamin A + D)
Cod Liver Oil (Vitamin A + D)

Dexibuprofen
Dexibuprofen

Diacerein + Glucosamine Sulphate
Diacerein + Glucosamine Sulphate

Diclofenac Sodium
Diclofenac Sodium

Diclofenac Sodium + Misoprostol
Diclofenac Sodium + Misoprostol

Diclofenac Sodium 1% Topical
Diclofenac Sodium 1% Topical

Duloxetine
Duloxetine

Esomeprazole + Naproxen
Esomeprazole + Naproxen

Etodolac
Etodolac

Etoricoxib
Etoricoxib

Glucosamine
Glucosamine

Ibuprofen
Ibuprofen

Indomethacin
Indomethacin

Mefenamic Acid
Mefenamic Acid

Meloxicam
Meloxicam

Menthol 10% + Methyl Salicylate 15% Topical
Menthol 10% + Methyl Salicylate 15% Topical

Menthol 10% + Methyl Salicylate 30% Topical
Menthol 10% + Methyl Salicylate 30% Topical

Methylprednisolone Sodium Succinate
Methylprednisolone Sodium Succinate

Naproxen 10% Topical
Naproxen 10% Topical

Oxaprozin
Oxaprozin

Paracetamol
Paracetamol

Salsalate
Salsalate

Sodium Hyaluronate
Sodium Hyaluronate

Sulindac
Sulindac

Tolmetin
Tolmetin

Tramadol Hydrochloride
Tramadol Hydrochloride

Valdecoxib
Valdecoxib

Rofecoxib
Rofecoxib

Nimesulide
Nimesulide

Bromelain + Trypsin
Bromelain + Trypsin

Aceclofenac
Aceclofenac

Acemetacin
Acemetacin

Capsaicin 0.025% topical
Capsaicin 0.025% topical

Celecoxib
Celecoxib

Chondroitin + Glucosamine
Chondroitin + Glucosamine

Cod Liver Oil (Vitamin A + D)
Cod Liver Oil (Vitamin A + D)

Dexibuprofen
Dexibuprofen

Diacerein + Glucosamine Sulphate
Diacerein + Glucosamine Sulphate

Diclofenac Sodium
Diclofenac Sodium

Diclofenac Sodium + Misoprostol
Diclofenac Sodium + Misoprostol

Diclofenac Sodium 1% Topical
Diclofenac Sodium 1% Topical

Duloxetine
Duloxetine

Esomeprazole + Naproxen
Esomeprazole + Naproxen

Etodolac
Etodolac

Etoricoxib
Etoricoxib

Glucosamine
Glucosamine

Ibuprofen
Ibuprofen

Indomethacin
Indomethacin

Mefenamic Acid
Mefenamic Acid

Meloxicam
Meloxicam

Menthol 10% + Methyl Salicylate 15% Topical
Menthol 10% + Methyl Salicylate 15% Topical

Menthol 10% + Methyl Salicylate 30% Topical
Menthol 10% + Methyl Salicylate 30% Topical

Methylprednisolone Sodium Succinate
Methylprednisolone Sodium Succinate

Naproxen 10% Topical
Naproxen 10% Topical

Oxaprozin
Oxaprozin

Paracetamol
Paracetamol

Salsalate
Salsalate

Sodium Hyaluronate
Sodium Hyaluronate

Sulindac
Sulindac

Tolmetin
Tolmetin

Tramadol Hydrochloride
Tramadol Hydrochloride

Valdecoxib
Valdecoxib

Rofecoxib
Rofecoxib

Nimesulide
Nimesulide

Bromelain + Trypsin
Bromelain + Trypsin