Overview Of Systemic hyperfibrinolysis
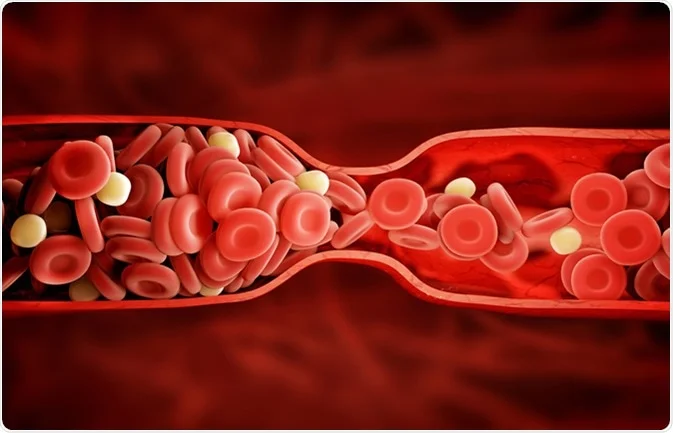
Systemic hyperfibrinolysis is a pathological condition characterized by the excessive breakdown of fibrin clots throughout the circulatory system. This hyperactivity of the fibrinolytic pathway results in an inability to maintain stable clots, leading to persistent or recurrent bleeding. It can be a standalone condition or secondary to other disorders such as trauma, surgery, malignancies, or disseminated intravascular coagulation (DIC).
Symptoms of Systemic hyperfibrinolysis
- - Persistent bleeding from surgical sites or injuries. - Easy bruising or hematomas without significant trauma. - Signs of shock in severe cases, such as hypotension, tachycardia, or pallor. - Microvascular bleeding manifesting as petechiae or mucosal bleeding.
Causes of Systemic hyperfibrinolysis
- - Trauma or Surgery: Massive injuries or surgical interventions can trigger a systemic release of plasminogen activators, leading to excessive clot degradation. - Sepsis or Infections: Inflammatory mediators in severe infections may activate the fibrinolytic system. - Malignancies: Certain cancers, particularly hematologic malignancies, can cause systemic fibrinolytic activation. - Liver Dysfunction: Impaired production of clotting and antifibrinolytic proteins contributes to this imbalance.
Risk Factors of Systemic hyperfibrinolysis
- - Severe Trauma: Especially when associated with massive blood transfusions or tissue damage. - Surgical Interventions: Complex procedures with extensive tissue manipulation. - Systemic Diseases: Including malignancies, liver disease, or sepsis.
Prevention of Systemic hyperfibrinolysis
- - Early recognition of trauma or surgical complications. - Prophylactic antifibrinolytics in high-risk situations, such as major surgeries or trauma with massive transfusions. - Close monitoring of coagulation parameters in critically ill patients.
Prognosis of Systemic hyperfibrinolysis
- The outcome depends on the underlying cause and the timeliness of intervention. Early and targeted treatment significantly improves recovery, while delayed intervention increases the risk of life-threatening bleeding complications.
Complications of Systemic hyperfibrinolysis
- - Hemorrhagic Shock: Resulting from uncontrolled systemic bleeding. - Organ Failure: Due to hypoperfusion from excessive blood loss. - DIC: Often coexists with or progresses from hyperfibrinolysis, exacerbating the bleeding tendency.
Related Diseases of Systemic hyperfibrinolysis
- - DIC: A coagulopathy marked by widespread clotting and secondary fibrinolysis. - Liver Disease: Impaired production of clotting and antifibrinolytic proteins exacerbates fibrinolytic activity. - Thrombocytopenia: Low platelet count complicating the hemostatic process.
Treatment of Systemic hyperfibrinolysis
Management involves addressing the underlying cause and restoring hemostatic balance: - **Antifibrinolytic Agents**: Drugs like tranexamic acid or epsilon-aminocaproic acid inhibit excessive fibrinolysis. - **Blood Product Replacement**: Fresh frozen plasma, cryoprecipitate, or platelets as needed. - **Supportive Measures**: Fluid resuscitation and hemodynamic stabilization in cases of significant blood loss.
Generics For Systemic hyperfibrinolysis
Our administration and support staff all have exceptional people skills and trained to assist you with all medical enquiries.

Aminocaproic Acid
Aminocaproic Acid

Aminocaproic Acid
Aminocaproic Acid